How Many Embryos To Make During IVF?
In vitro fertilization (IVF) is a complex process that involves multiple steps with various decisions. One important “decision” along the journey is how many embryos to create.
The number of embryos you make can significantly impact the success rates and risks associated with the procedure.
In this article, we’ll explore the factors influencing the decision of how many embryos to make during IVF, including patient age, embryo quality, whether or not the embryos are PGT tested, and individual health circumstances. Keep in mind the statistics we cite in this article are averages. It’s essential to assess your individual fertility factors and goals with your specialist before letting statistics dictate your hope.
How Many Embryos Should You Make?
The question of how many embryos you should make has much to do with your age and protocol/gonadotropin dosage. Fertility, and therefore IVF success rates per embryo transfer, decline rapidly for women over 35.
Age impacts the number of embryos you should aim for because embryos created from the eggs of older women are much more prone to genetic and chromosomal abnormalities. At the same time, for women of late maternal age, creating more embryos is often more difficult because there are fewer eggs and the body does not respond as well to fertility medications.
Let’s take a closer look at what the research tells us about the various factors that inform how many embryos a woman should expect to make in order to give herself the greatest likelihood of a successful live birth.
How Many Embryos Can You Expect to Make?
The number of embryos that you can expect during in vitro fertilization (IVF) depends on a complex combination of factors, including age, ovarian reserve, the quality of your eggs, and the presence of underlying conditions such as PCOS and endometriosis.
That said, here’s a rough breakdown of how many embryos one might expect based solely on age.
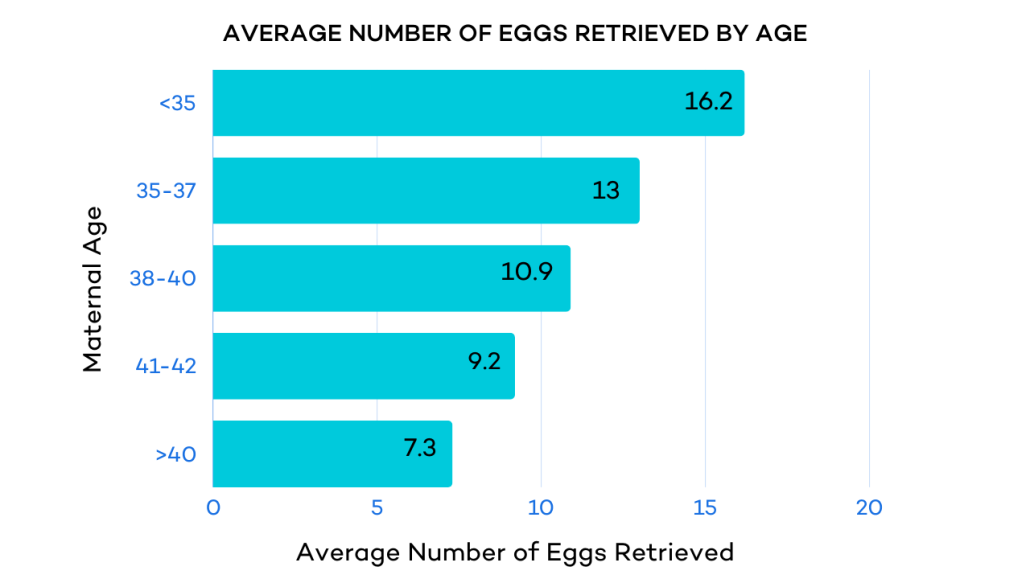
On average, 5-20 eggs are retrieved per IVF cycle. As with all IVF stages, age has the most significant impact.
Keep in mind that the number of eggs retrieved does not equal the number of embryos. As with each IVF stage, there is an expected rate of attrition.
Age 20-29
- 70% of mature eggs fertilize
- 70% of those that fertilize make it to cleavage (day 3)
- 50% make it to blastocyst
Age 30-39
- 70% of mature eggs fertilize
- 50% make it to cleavage (day 3); of those
- 40-50% make it to blastocyst
Age 40 and older
- 70% Fertilize–No meaningful statistics thereafter.
Cleavage-stage embryos have a slightly lower live birth rate (31%) after transfer than blastocyst-stage embryos (32-41%).5
If we combine the above data, we get roughly 8 embryos per retrieval for women under 35, and between 4-5 embryos for women aged 35-40.
IVF Success Rates Per Embryo Transfer
The Society for Reproductive Technology (SART) states that for women under 35 without undergoing genetic testing, the overall percentage of live births from one IVF Cycle/Retrieval (including all transfers) is 55.6%.

For this broad age group, live birth rates per single embryo transfer were 41.4%, and for subsequent transfers, it’s around 47%.
After 5 embryos were transferred, the average cumulative live birth rate was 52%, with approximately a 10% relative increase in cumulative live birth rate per additional embryo, reaching a maximum 69% live birth rate per person with 5 embryos.
The research also shows a 3.4% increase in success per embryo up to a total of 10 embryos, achieving a cumulative pregnancy rate of 79%.
For 10-15 embryos, the increased live birth rate drops to a 2% increase in CLBR per embryo.
General Recommendations for How Many Embryos To Make During IVF
Based on the population-based statistics above, it is difficult to determine how many embryos any one individual should try to make. There are many factors that are simply not in a patient’s control.
But if we are to follow the averages, we find that the optimal minimum number of embryos to make during IVF varies depending on individual circumstances, such as age, goal family size, and embryo quality. Here’s the breakdown:
For Women 35 and Younger
- Aim to create and transfer at least three chromosomally normal embryos, if feasible, to maximize the chances of pregnancy via IVF.
- Creating additional embryos for subsequent transfers can increase the chances of success.
For Women Older Than 35
- Creating more embryos can be beneficial but challenging due to lower success rates per embryo at advanced maternal age.
- If the embryos undergo PGT genetic testing, the success rate is similar to non-tested embryos in younger women: approximately 65% on the first “normal” euploid embryo transfer, 88% on the second euploid embryo transfer, and 95% by the 3rd euploid embryo transfer.
- For women over 35 or with known fertility issues, transferring more embryos may be advisable, balancing the increased cumulative live birth rate against the risk of multiple pregnancies.
Other Reasons for Creating and Freezing Multiple Embryos
In addition to considering how many embryos to make and transfer during a current IVF cycle, many patients elect to create and freeze multiple embryos for various reasons. These include:
Future Family
Many people choose to delay childbirth for social, personal, and professional reasons. As egg quality and fertility decline sharply in the mid to late thirties, creating and freezing embryos is an effective way to extend a woman’s biological clock.
Cancer
Women receiving chemotherapy or pelvic radiation for cancer have a high risk of fertility issues. Creating and freezing embryos before treatment can significantly reduce these risks.
Transitioning
Hormone therapy for transitioning will result in infertility. Creating and freezing embryos before transitioning can preserve one’s ability to reproduce.
Premature Ovarian Failure
Some women are at risk of premature ovarian failure due to chromosomal abnormalities, such as Turner syndrome or Fragile X syndrome, or a family history of early menopause. Freezing embryos at a younger age can help preserve fertility before it diminishes significantly.
Surgeries
Various surgeries can put a woman’s ovaries at risk of being damaged. In some cases, the ovaries must be surgically removed because of genetic disorders. Freezing embryos before certain surgeries can protect one’s fertility.
How Many Embryos Should You Make During IVF: The Bottom Line
In vitro fertilization (IVF) is a multi-step process that requires careful consideration at each step, especially when deciding on the number of embryos to create. The success rates and associated risks can vary based on factors such as your age, egg quality, embryo quality, and individual health circumstances.
Research indicates that younger women have higher success rates with fewer embryos, while older women may benefit from creating more embryos due to a natural decline in fertility. Utilizing preimplantation genetic testing (PGT) can also enhance success rates by ensuring the transfer of chromosomally normal embryos.
Ultimately, the number of embryos that one makes is a personalized decision that includes consideration of each patient’s unique fertility factors and medical conditions.
If you’re ready to explore the best choices for your IVF journey, schedule a consultation with one of our specialists today.



