How Many Embryos to Transfer in IVF: Guidelines and Factors

Determining how many embryos to transfer is a critical decision in the IVF process. This choice impacts your chances of pregnancy and the chance of multiple births, which can pose health risks to both the mother and the babies.
The number of embryos to transfer is influenced by various factors, including the patient’s age at the time the eggs were retrieved, embryo quality and genetic testing, and previous IVF outcomes.
Current medical guidelines and assessments of your personal care needs are aimed at balancing the best chances for a successful pregnancy with the safety of both the mother and potential babies.
In this article, we’ll help you understand these considerations so you can better navigate the complex landscape of IVF treatment.
Current Guidelines for How Many Embryos to Transfer
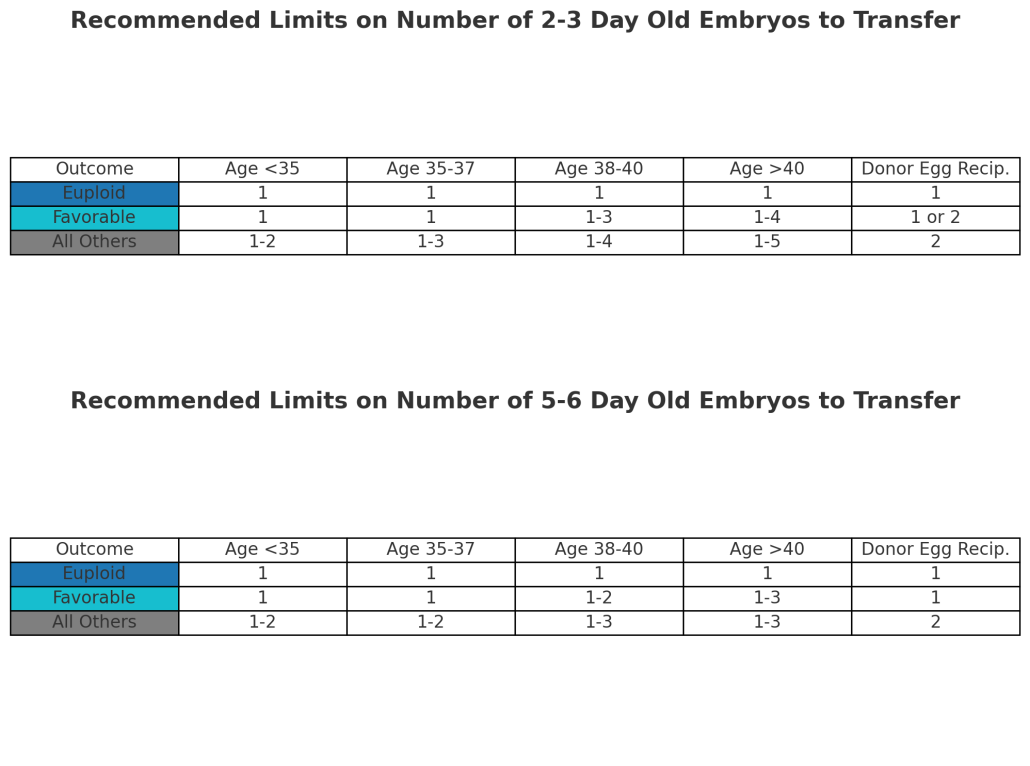
Here are the guidelines from the American Society for Reproductive Medicine for how many embryos to transfer per IVF cycle: 1
- Euploid (chromosomally normal) embryo: Only one euploid embryo should be transferred, regardless of the patient’s age.
- Patients under 35 years old are strongly advised to opt for a single-embryo transfer, regardless of whether the embryo is at the cleavage or blastocyst stage.
- Patients aged 35-37 years are strongly advised to undergo a single-embryo transfer.
- Patients aged 38-40 years are advised to transfer no more than three untested cleavage-stage embryos or two blastocysts.
- Patients aged 41-42 years are to limit transfers to no more than four untested cleavage-stage embryos or three blastocysts.
For each of these age groups, patients who do not qualify for a favorable prognosis might be eligible for the transfer of an additional embryo based on their specific situation.
Be aware that there is an increased chance of getting pregnant with two or more children with a multiple transfer and that twin or higher order pregnancies carry greater risk to the mother and fetuses.
If you’re a patient with an otherwise favorable prognosis but do not successfully conceive after several cycles with high-quality embryos, your physicians might consider transferring an additional embryo or adding additional testing.
Finally, patients with medical conditions that could lead to significant complications from multiple gestation pregnancies should limit the transfer to a single embryo.
Success Rates for Tested vs. Untested Embryos By Age
Using preimplantation genetic testing (PGT) to determine if an embryo is chromosomally “normal” can significantly impact its success rates and, therefore, may influence your choice of how many embryos to make and transfer.
Chances of a single, untested embryo resulting in a live birth [15]:
- 41% for women under age 35
- 30% for women ages 35-37
- 20% for women ages 38-40
- 10-12% for women ages 41-42
- 5% for women ages 43-44
- Less than 1% for women over 44
PGT-A Tested Embryos
PGT-A testing can help increase the chances of success per embryo transfer by identifying normal and abnormal embryos and ensuring the embryo(s) being transferred have the correct number of chromosomes.
A 2018 study evaluating the effectiveness of SNP-based Preimplantation Genetic Testing for Aneuploidy (PGT-A) over 1621 IVF cycles yielded the following insights :
Clinical Pregnancy rate (%) | For all ages | <35 | 35-37 | 38-40 | 41-42 | >42 | All ages with donor eggs |
Overall, per embryo | 70.6 | 70.4 | 76.6 | 65.9 | 65.3 | 72.2 | 64.8 |
Per single embryo transfer | 68.6 | 67.2 | 75.0 | 64.8 | 65.2 | 72.2 | 62.3 |
Per double embryo transfer | 81.9 | 81.7 | 86.7 | 78.3 | 66.7 | ND | 78.3 |
Clinical Pregnancy rate (%) | For all ages | <35 | 35-37 | 38-40 | 41-42 | >42 | All ages with donor eggs |
Overall, per embryo transfer | 64.5 | 65.6 | 71.3 | 59.5 | 49.0 | 72.2 | 52.4 |
Single embryo transfer | 61.7 | 61.0 | 68.8 | 58.6 | 47.8 | 72.2 | 48.4 |
Double embryo transfer | 77.6 | 80.0 | 83.3 | 65.2 | 66.7 | ND | 73.9 |
Across all age groups, the clinical pregnancy rates are relatively high when using PGT-A tested embryos, averaging around a 69% live birth rate. This indicates that PGT-A testing is effective in identifying viable embryos, thereby increasing the chances of a successful live birth per embryo transfer.
Success Rates Per Embryo Grade
A 2017 study assessing 1,700 single embryo transfers found a relationship between embryo grades and implantation rates:
- “Good” embryos had a 55% implantation rate, and a 46.8% birth rate.
- “Fair” embryos had a 47.2% implantation rate, and a 39% birth rate.
- “Poor” embryos had a 43.6% implantation rate, and a 34.1% birth rate
Keep in mind that embryo grading is a highly subjective process. Grading involves making a subjective designation based on a picture of the embryo that may be of poor quality or show only a single side of the embryo.
A “poor” graded embryo still has a 1 in 3 chance of resulting in a live birth. This is reflected in the general recommendations to create at least 2-3 chromosomally normal embryos per child desired regardless of grade.
How Many Embryos to Transfer During IVF: The Take Away
Determining the optimal number of embryos to transfer in IVF involves balancing the chances of pregnancy with the risks of multiple births. To minimize complications, guidelines recommend single embryo transfers (SET) for most patients, especially those under the age of 38. Double embryo transfers (DET) are generally only considered for older patients or those with previous IVF failures who have not done genetic testing of embryos.
Preimplantation genetic testing for aneuploidy (PGT-A) significantly improves success rates by selecting chromosomally normal embryos for transfer, which can mitigate natural age related declines for patients of later maternal age.
Embryo grading is another protocol that can help you choose which embryos to transfer, but it is a highly subjective process that only modestly improves success rates.
The takeaway here is that the number of embryos to transfer is one for most patients, but it is ultimately a personalized decision that considers age, genetic testing results, and individual risk factors to optimize your chances of a healthy pregnancy.



