ICSI vs. IVF: What’s the Difference?
In Vitro Fertilization (IVF) is the most effective assisted reproductive technology used to establish a pregnancy. IVF is a complex and multistage process in which eggs are retrieved from the ovary(ies), fertilized with sperm in a lab, grown to an embryo, and then an embryo is placed back into the uterus. IVF is most commonly used for people experiencing infertility, but it may also be used by same-sex couples or those looking to choose the biological sex of their child.
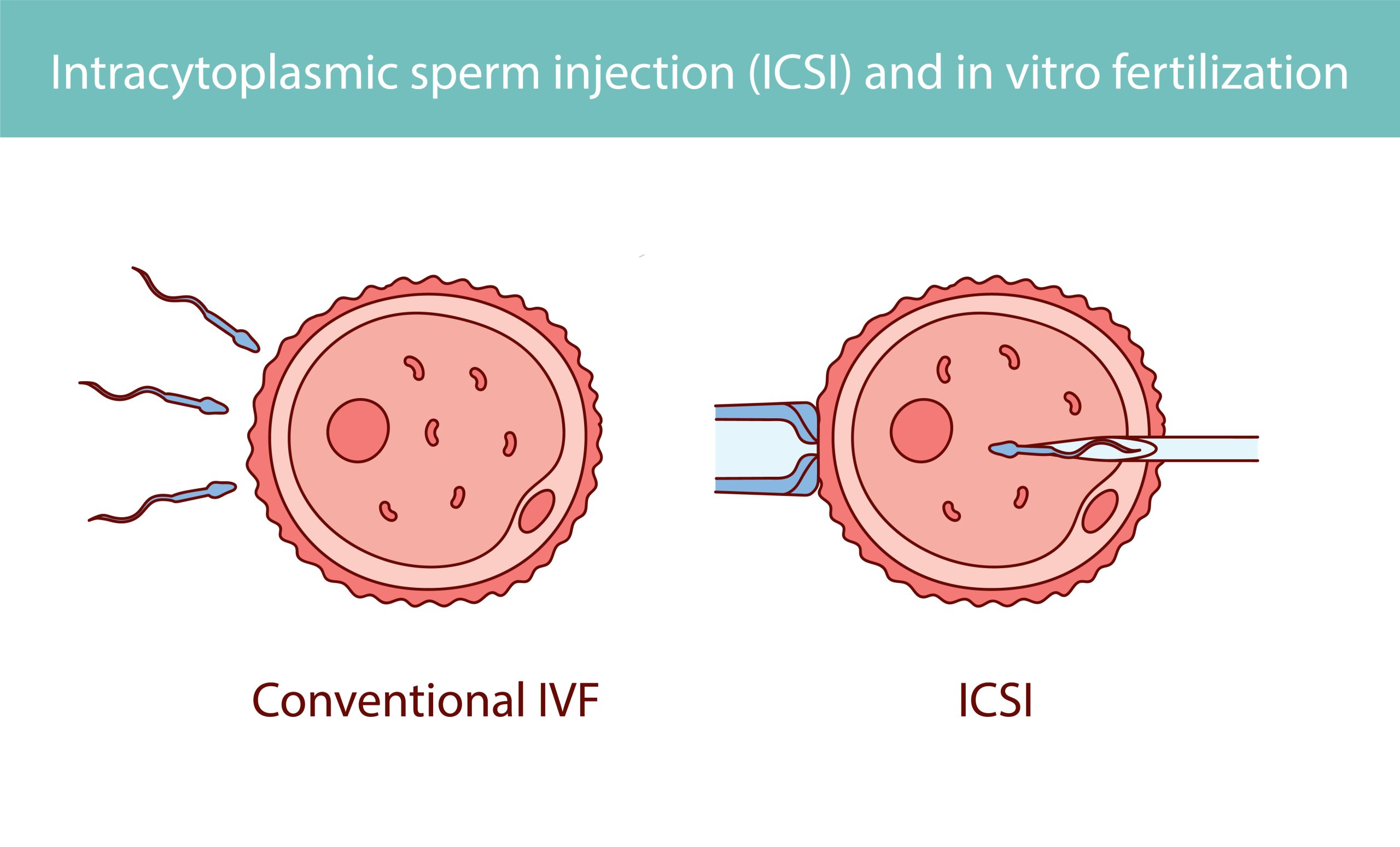
In IVF, there are two potential fertilization methods: Intracytoplasmic Sperm Injection (ICSI) and Conventional IVF.
Conventional IVF is designed to address female infertility issues, such as blocked fallopian tubes or endometriosis, whereas ICSI was developed primarily to treat male infertility issues, like low sperm count or immotility. However, as of 2012, ICSI is used in at least 76% of all IVF cycles regardless of male or female factor infertility.
This article will explore these two common fertilization methods with In Vitro Fertilization, including what they are, why they were developed, who they are for, success rates, and more.
Conventional IVF: Process and Use
“Conventional IVF” follows the meaning of “In Vitro,” a process performed or taking place in a test tube or culture dish. It involves placing eggs in petri dish along with a culture medium and sperm. From there, the sperm fertilizes the egg in a relatively natural fashion. The sperm must swim to the egg, bind to and penetrate the egg’s outer layer, known as the zona pellucida, to trigger the fertilization process.
This is the process that was used to fertilize the egg in both the first non-human IVF in 1959 and the successful first human IVF in 1978.
While developed over a half-century ago, this method of fertilization is still commonly used when male infertility is not a primary concern.
ICSI: A Focus on Male Infertility
ICSI is a more recent advancement, developed primarily to help with male infertility.
In this method, instead of relying on sperm to fertilize the egg naturally, an embryologist directly injects a single sperm into the egg using a microscopic needle.
ICSI is especially useful for men with low sperm count (oligozoospermia) or poor sperm motility (asthenozoospermia). It has since become a widely used procedure in many fertility clinics, even in cases where male infertility isn’t the issue.
Success Rates: ICSI vs. Conventional IVF
On average, ICSI successfully fertilizes 50-80% of injected eggs, while conventional IVF fertilizes around 50% of eggs. However, it’s important to note that fertilization rates don’t directly translate into clinical pregnancy or live birth rates.
Once fertilization has occurred, the chances of pregnancy with ICSI are comparable to those with conventional IVF. For cases involving male infertility, ICSI can be a highly effective solution, whereas studies show that in cases without male infertility, ICSI and traditional IVF offer similar success rates.
Choosing Between ICSI and Conventional IVF
The decision to use ICSI or conventional IVF depends on the couple’s individual circumstances and the fertility clinic’s operational protocols. Factors like sperm and egg quality, the number of eggs available, and the cause of infertility all play a role.
When only a limited number of eggs are available, ICSI is often preferred because it allows for the careful selection of the best sperm. On the other hand, when donor sperm or eggs are used, ICSI may not be necessary due to the high quality of the donor gametes.
Even if ICSI is not “needed,” some fertility clinics, including CNY, consider it the standard of care and perform ICSI across the board unless specifically asked not to by the patient.
Similarities Between ICSI and Conventional IVF
Regardless of whether ICSI or conventional IVF is chosen, the IVF processes leading up to and following fertilization are the same.
Both techniques involve ovarian stimulation and egg retrieval. The embryos are cultured in the lab for 2-6 days before being transferred to the uterus or frozen in storage for later use to establish a pregnancy.
Cost
The average cost of intracytoplasmic sperm injection (ICSI) is around $1,500. However, this too is highly variable. Some clinics include ICSI in their base pricing, while others charge upwards of $3,000. Here at CNY, we include the price of ICSI as the standard of care for our IVF cycles.
IVF vs. ICSI: The Takeaway
At CNY Fertility, ICSI is the default standard of care and is used in the majority of cases (over 99%) to minimize the risk of fertilization failure.
However, both ICSI and conventional IVF are available options, and the best choice depends on the unique needs of each patient as determined by you and your fertility specialist.
To learn if ICSI or conventional IVF is right for you, schedule a consultation today.