The IVF Funnel: Rates of Attrition in the IVF Process
The IVF Funnel refers to the reduction in viable options as one progresses through the IVF process. That is:
- _ number of follicles detected during simulation
- _ number of eggs retrieved
- _ number of mature eggs retrieved
- _ number of eggs successfully fertilized
- _ number of cleavage stage embryos
- _ number of blastocyst stage embryos
- _ number of PGT tested normal embryos (optional)
- _ number of embryos transferred
- _ number of positive pregnancy tests
- _ number of fetal heartbeats detected
- _ number of live births
- _ number of embryos remaining for future Frozen Embryo Transfers.
It’s important to know that the reduction of “options” as one progresses through IVF is completely normal. As such, understanding the IVF funnel can be an incredibly empowering way to manage expectations while staying hopeful.
In this article, we’ll provide examples of typical passages through the IVF funnel and also provide important details at each of the key stages so you can have a better understanding of what the number of follicles, eggs, embryos, and transfers means. Wherever you are in the IVF process, we hope this article serves as a beacon of clarity.
Key points when starting out
IVF treatment involves a series of complex medication, surgical, and laboratory techniques. A significant proportion of eggs and embryos will not make it through to successive stages. The numbers presented in this article and success rates of IVF are HIGHLY variable and strongly influenced by the age of the person when eggs are retrieved, underlying medical conditions, medication protocols, and more.
Let’s explore each of the stages of the IVF funnel and how they impact the chances of a successful live birth.
10 Examples of The IVF Funnel
Example 1:
- 20 follicles in both ovaries (detected during monitoring appointments during ovarian stimulation)
- 16 mature follicles in both ovaries (at final monitoring appointment during ovarian stimulation)
- 19 eggs retrieved from the follicles; 16 mature eggs retrieved (At initial inspection of eggs in embryology lab)
- 14 mature eggs successfully fertilized with sperm (at fertilization check “day 1” – the day after egg retrieval)
- 12 cleavage (day-3) embryos
- 8 blastocyst (day-5) embryos
- 6 embryos found to be chromosomally normal after preimplantation genetic testing
- 2 embryo transfers attempted
- 2 positive pregnancy tests are achieved
- 1 pregnancy confirmed via fetal heartbeat
- 1 full-term pregnancy and live birth
- 4 embryos frozen for future Frozen Embryo Transfers
Example 2:
- 40 follicles in both ovaries (detected during monitoring appointments during ovarian stimulation)
- 10 mature follicles in both ovaries (at final monitoring appointment during ovarian stimulation)
- 20 eggs retrieved from the follicles; 9 mature eggs retrieved (At initial inspection of eggs in embryology lab)
- 8 mature eggs successfully fertilized with sperm (at fertilization check “day 1” – the day after egg retrieval)
- 6 cleavage (day-3) embryos
- 3 blastocyst (day-5) embryos
- 2 embryos found to be chromosomally normal after preimplantation genetic testing
- 1 embryo transfer attempted
- 1 positive pregnancy tests are achieved
- 1 pregnancy confirmed via fetal heartbeat
- 1 full-term pregnancy and live birth
- 1 embryos frozen for future Frozen Embryo Transfers
Example 3: Healthy 40-year-old woman
- 5 follicles in both ovaries (detected during monitoring appointments during ovarian stimulation)
- 2 mature follicles in both ovaries (at final monitoring appointment during ovarian stimulation)
- 2 eggs retrieved from the follicles; 2 mature eggs retrieved (At initial inspection of eggs in embryology lab)
- 2 mature eggs successfully fertilized with sperm (at fertilization check “day 1” – the day after egg retrieval)
- 1 cleavage (day-3) embryos (transferred at day 3)
- 0 blastocyst (day-5) embryos
- _ embryos found to be chromosomally normal after preimplantation genetic testing – Not Applicable
- 1 embryo transfer attempted
- 1 positive pregnancy tests are achieved
- 1 pregnancy confirmed via fetal heartbeat
- 1 full-term pregnancy and live birth
- 0 embryos frozen for future Frozen Embryo Transfers
Example 4:
- 20 follicles in both ovaries (detected during monitoring appointments during ovarian stimulation)
- 16 mature follicles in both ovaries (at final monitoring appointment during ovarian stimulation)
- 22 eggs retrieved from the follicles; 20 mature eggs retrieved (At initial inspection of eggs in embryology lab)
- 17 mature eggs successfully fertilized with sperm (at fertilization check “day 1” – the day after egg retrieval)
- 15 cleavage (day-3) embryos
- 12 blastocyst (day-5) embryos
- 4 embryos found to be chromosomally normal after preimplantation genetic testing
- 3 embryo transfers attempted
- 3 positive pregnancy tests are achieved
- 2 pregnancies confirmed via fetal heartbeat
- 1 full-term pregnancy and live birth
- 1 embryos frozen for future Frozen Embryo Transfers
Example 5:
- 5 follicles in both ovaries (detected during monitoring appointments during ovarian stimulation)
- 8 mature follicles in both ovaries (at final monitoring appointment during ovarian stimulation)
- 17 eggs retrieved from the follicles; 15 mature eggs retrieved (At initial inspection of eggs in embryology lab)
- 12 mature eggs successfully fertilized with sperm (at fertilization check “day 1” – the day after egg retrieval)
- 8 cleavage (day-3) embryos
- 5 blastocyst (day-5) embryos
- _ embryos found to be chromosomally normal after preimplantation genetic testing – Not Applicable
- 1 embryo transfer attempted
- 1 positive pregnancy tests are achieved
- 1 pregnancy confirmed via fetal heartbeat
- 1 full-term pregnancy and live birth
- 4 embryos frozen for future Frozen Embryo Transfers
Example 6:
- 10 follicles in both ovaries (detected during monitoring appointments during ovarian stimulation)
- 5 mature follicles in both ovaries (at final monitoring appointment during ovarian stimulation)
- 6 eggs retrieved from the follicles; 4 mature eggs retrieved (At initial inspection of eggs in embryology lab)
- 3 mature eggs successfully fertilized with sperm (at fertilization check “day 1” – the day after egg retrieval)
- 2 cleavage (day-3) embryos
- _ blastocyst (day-5) embryos – not applicable – blastocyst transfer not attempted
- _ embryos found to be chromosomally normal after preimplantation genetic testing – not applicable
- 1 embryo transfers using both embryos attempted
- 1 positive pregnancy tests are achieved
- 1 fetal heartbeat detected
- 1 full-term pregnancy and live birth
- 0 embryos frozen for future Frozen Embryo Transfers
Example 7:
- 15 follicles in both ovaries (detected during monitoring appointments during ovarian stimulation)
- 12 mature follicles in both ovaries (at final monitoring appointment during ovarian stimulation)
- 10 eggs retrieved from the follicles; 9 mature eggs retrieved (At initial inspection of eggs in embryology lab)
- 7 mature eggs successfully fertilized with sperm (at fertilization check “day 1” – the day after egg retrieval)
- 5 cleavage (day-3) embryos
- 3 blastocyst (day-5) embryos
- _ embryos found to be chromosomally normal after preimplantation genetic testing (not applicable)
- 1 embryo transfer attempted
- 1 positive pregnancy tests are achieved
- 1 pregnancy confirmed via fetal heartbeat
- 1 full-term pregnancy and live birth
- 2 embryos frozen for future Frozen Embryo Transfers
Example 8:
- 25 follicles in both ovaries (detected during monitoring appointments during ovarian stimulation)
- 20 mature follicles in both ovaries (at final monitoring appointment during ovarian stimulation)
- 18 eggs retrieved from the follicles; 15 mature eggs retrieved (At initial inspection of eggs in embryology lab)
- 12 mature eggs successfully fertilized with sperm (at fertilization check “day 1” – the day after egg retrieval)
- 9 cleavage (day-3) embryos
- 8 blastocyst (day-5) embryos
- 6 embryos found to be chromosomally normal after preimplantation genetic testing
- 2 embryo transfers attempted
- 2 positive pregnancy tests are achieved
- 1 pregnancy confirmed via fetal heartbeat
- 1 full-term pregnancy and live birth
- 4 embryos frozen for future Frozen Embryo Transfers
Example 9:
- 50 follicles in both ovaries (detected during monitoring appointments during ovarian stimulation)
- 25 mature follicles in both ovaries (at final monitoring appointment during ovarian stimulation)
- 30 eggs retrieved from the follicles; 20 mature eggs retrieved (At initial inspection of eggs in embryology lab)
- 10 mature eggs successfully fertilized with sperm (at fertilization check “day 1” – the day after egg retrieval)
- 5 cleavage (day-3) embryos
- 2 blastocyst (day-5) embryos
- _ embryos found to be chromosomally normal after preimplantation genetic testing (not applicable)
- 2 embryo transfers attempted
- 1 positive pregnancy tests are achieved
- 1 pregnancy confirmed via fetal heartbeat
- 1 full-term pregnancy and live birth
- 0 embryos frozen for future Frozen Embryo Transfers
Example 10: Example 10:
- 13 follicles in both ovaries (detected during monitoring appointments during ovarian stimulation)
- 5 mature follicles in both ovaries (at final monitoring appointment during ovarian stimulation)
- 7 eggs retrieved from the follicles; 6 mature eggs retrieved (At initial inspection of eggs in embryology lab)
- 6 mature eggs successfully fertilized with sperm (at fertilization check “day 1” – the day after egg retrieval)
- 5 cleavage (day-3) embryos
- 3 blastocyst (day-5) embryos
- 1 embryos found to be chromosomally normal after preimplantation genetic testing (not applicable)
- 1 embryo transfers attempted
- 1 positive pregnancy tests are achieved
- 1 pregnancy confirmed via fetal heartbeat
- 1 full-term pregnancy and live birth
- 0 embryos frozen for future Frozen Embryo Transfers
Example take aways
IVF patients usually start with a higher number of follicles, which reduce in number as the patient makes their way through the IVF funnel. That said, follicular ultrasounds may not always show an accurate picture, so patients often end up with more or less mature eggs at retrieval than what is measured via ultrasound at their final monitoring appointment.Step 1 of the IVF Funnel: Follicle Count (Stimulation and Monitoring)
The first stage of the IVF funnel begins with ovarian stimulation. During this phase, the patient undergoes hormonal therapy for 7-14 days to stimulate the ovaries to produce multiple mature eggs in her ovaries.
Typically, this involves daily self-administered injections of follicle-stimulating hormone (FSH) and sometimes letrozole, clomid, and luteinizing hormone (LH). During this period, your doctor will closely monitor the stimulation using ultrasound and blood tests to measure the number and size of follicles. Ovarian follicles are small fluid-filled sacks in which the eggs develop. Follicles over 16 mm are considered to be mature. Generally, 90+% of mature follicles yield an egg. [1]
Though the goal of the stimulation period is to develop as many mature follicles as possible, the outcome is highly dependent upon the patient’s age and AMH level, along with various other factors and diagnoses.
Though your doctor uses ultrasound to get a rough idea of your number of follicles, ultrasound imaging is imprecise and is not considered to be an accurate assessment of the actual number of follicles and eggs you will have at the time of retrieval.
For example, someone could have 10 mature follicles at the time of their last monitoring appointment, but during the egg retrieval find 15 mature follicles. Alternatively someone could appear to have 10 follicles at their last monitoring appointment, but only be able to aspirate 5 mature follicles at the time of egg retrieval.
Step 2 of the IVF Funnel: Number of Eggs (at Egg Retrieval)
When the follicles reach a size of maturation, egg retrieval is performed. During the egg retrieval, the patient is sedated, and a thin needle is used to extract the fluid from the mature follicles under ultrasound guidance. Your eggs are in this fluid. [2]
Retrieving multiple eggs increases your chances of successful fertilization and pregnancy. [3] However, there is a limit to the more is better outlook. At a certain point, having too many eggs may indicate ovarian hyperstimulation, which can lead to an overall lower quality of eggs and, therefore, a reduced live birth success rate.
A 2023 study looking at 172,341 IVF cycles found that the groups of people who retrieved 6-15 and 16-25 eggs had the highest rates of achieving a live birth, with the 16-25 eggs group having only a small increase over the 6-15 group. Whereas people who retrieved 1-5 eggs had a 47% lower live birth rate, and people who retrieved more than 25 eggs had a 42% lower live birth rate than the “average” 6-15 eggs group. [4]
Having an extremely high number of eggs is often an indication of PCOS or ovarian hyperstimulation, which can lead to overall lower-quality eggs and, therefore, lower success rates. [5] [6]
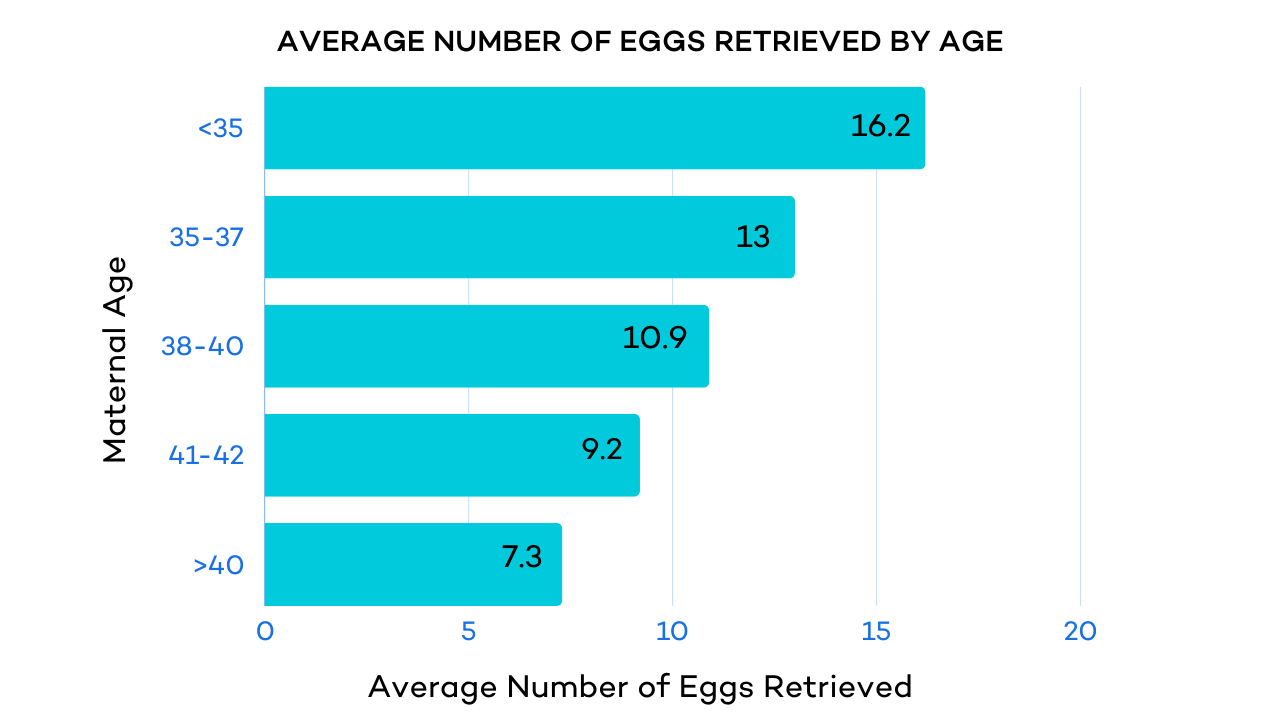
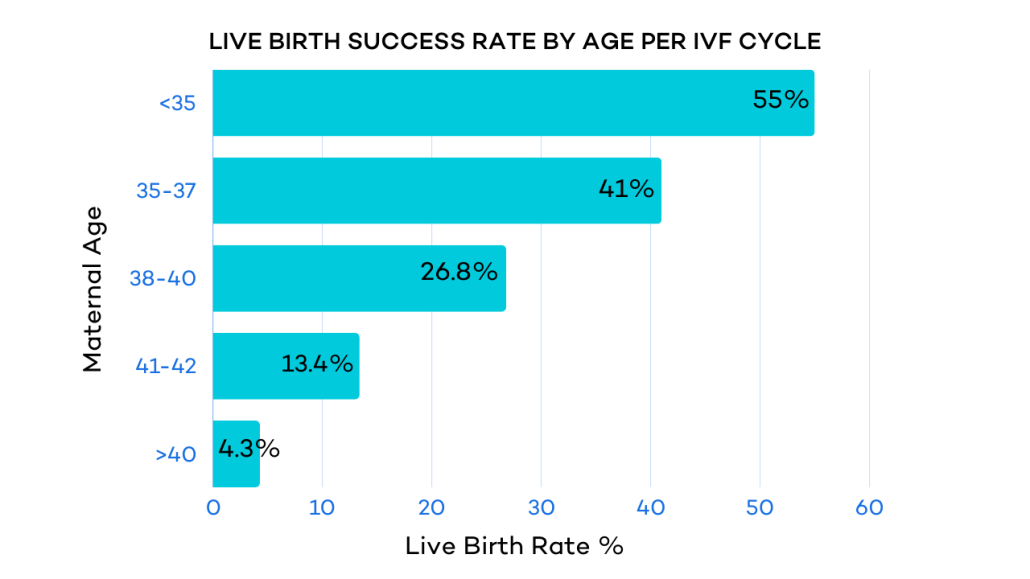
Age is another factor that can impact the number and quality of eggs retrieved and, therefore, the probability of a successful live birth.
For example, a 2013 study found that “In women age 35–39, optimal pregnancy rates (34.8%) were achieved with 5–9 eggs at retrieval. Less than 5 eggs significantly reduced the pregnancy rate (15.6%), whereas more than 10 eggs yielded pregnancy rates between 28 and 29%. In women over 40, we found a stepwise improvement in pregnancy rates with increased number of eggs at retrieval (1–4: 11%, 5–9: 21%, 10–14: 26%, 15–19: 33%).” [7]
Once retrieved, an embryologist will check to see if each egg is mature. It’s normal to have eggs that are not mature along with mature eggs.
Key points for step 2
On average, 5-20 eggs are retrieved during this stage.
The number of retrieved eggs does not equal the number of viable embryos or successful live births.
Both the number of eggs, quality of eggs, and the age of the patient impact the live birth success rate.
There is generally a decrease in the quantity of eggs retrieved as you get older.
Step 3: Number of Embryos (At fertilization check – day 1 after fertilization)
An embryologist will fertilize your eggs with sperm. This is commonly done by one of two methods: Injecting individual sperm directly into each egg through a process called intracytoplasmic sperm injection (ICSI). Or conventional fertilization, where many sperm are added to a petri dish containing the egg(s).
Key points for step 3
- At this stage, between 70-80% of mature eggs successfully fertilize.
- If sperm or egg quality is known to be low, the rate of fertilization can decrease.
Step 4: Cleavage Stage Embryos (Day 3 After Fertilization)
After fertilization, the egg becomes an embryo that reaches either the cleavage or blastocyst stage before it is implanted back into the uterus or frozen for future use. An embryo enters the cleavage stage 2-3 days after fertilization and typically has between 2 and 128 cells. [8] [9]
Age 20-29
- 70% of those that fertilize make it to cleavage (day 3)
- 50% make it to blastocyst
Age 30-39
- 50% make it to cleavage (day 3); of those
- 40-50% make it to blastocyst
Age 40 and older
- 70% Fertilize–No meaningful statistics thereafter
Key points for step 4
As with each stage, be prepared for normal levels of attrition. Overall, only 30-50% of fertilized eggs (embryos) will make it to the blastocyst stage.Stage 5 (Optional): Blastocyst Embryos (Day 5, 6, or 7 After Fertilization)
After being in the incubator for 5-7 days, an embryo undergoes cell divisions and can reach the blastocyst stage.
As a blastocyst, the embryo has two distinct parts: An outer layer called the trophectoderm that will eventually become the placenta, and the inner cell mass that will become the fetus. [10]
Once an egg reaches the blastocyst stage, it can be graded by an embryologist. These grades help identify which embryos should be prioritized for transfer and/or freezing.
Here’s a breakdown of the rates of successful fertilization for each age group.
Age 20-29
- 50% of embryos that make it to cleavage will make it to blastocyst
Age 30-39
- 40-50% of embryos that make it to cleavage will make it to blastocyst
Age 40 and older
- No meaningful statistics after fertilization
Key points for step 5
As with each stage, be prepared for normal levels of attrition. Overall, only 30-50% of fertilized eggs (embryos) will make it to the blastocyst stage.Summary of Stages 3-5:
Age 20-29
- 70% of mature eggs fertilize
- 70% of those that fertilize make it to cleavage (day 3)
- 50% make it to blastocyst
Age 30-39
- 70% of mature eggs fertilize
- 50% make it to cleavage (day 3); of those
- 40-50% make it to blastocyst
Age 40 and older
- 70% Fertilize–No meaningful statistics thereafter
Key points for step 3-5
- As with each stage, be prepared for normal levels of attrition. Overall, only 30-50% of fertilized eggs (embryos) will make it to the blastocyst stage.
- When transferring fresh embryos, 31% of women achieve a live birth after the transfer of a cleavage embryo, while 32-41% of women achieve a live birth after the transfer of a blastocyst-stage embryo.5
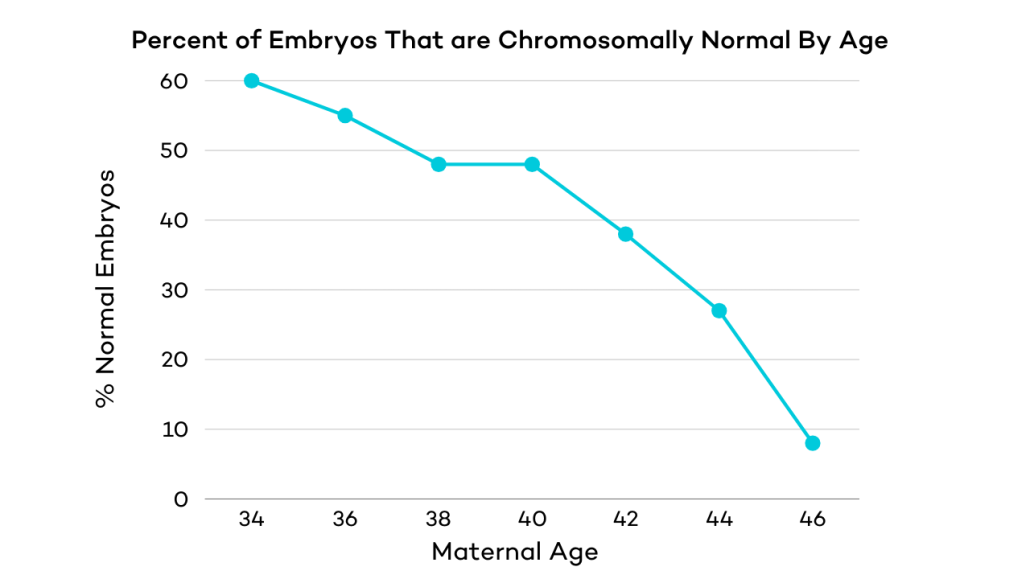
Step 6 (optional): Chromosomally Normal Embryos (Results After Genetic Testing)
At the blastocyst stage, a tissue biopsy can be taken from the embryo and tested for chromosomal abnormalities (basically, ensuring the embryo has the correct number of chromosomes) and/or if you want to choose the sex of your child.
Preimplantation genetic testing (PGT) is common for people who have a long history of infertility and pregnancy loss, those over 35, and for those at risk of known genetic diseases or chromosomal issues.
Testing can avoid implanting eggs with genetic abnormalities.
Key points for step 6
- As your age increases, the percentage of chromosomally normal embryos decreases
- Around 50% of eggs are chromosomally normal for women 35 years of age
- Only 10-15% of eggs are chromosomally normal for a woman aged 40
Step 7 of the Funnel: Embryo Implantation from Embryo Transfer
Embryos are transferred either fresh or frozen. A fresh transfer takes place approximately 14-20 days after the start of IVF medications, which is typically 3-7 days after the egg retrieval.
With a fresh transfer, usually 1-2 embryos are transferred while the rest (if any) are frozen. You can use the frozen embryos later if the fresh transfer isn’t successful or if you want to have more children. With a frozen transfer all fertilized eggs are frozen at the cleavage or blastocyst stage and transferred during a subsequent menstrual cycle.
Key points for step 7
- A fresh or frozen embryo transfer cannot guarantee a successful live birth and may necessitate multiple transfers.
- The proportion of transferred embryos that implant and result in at least a fetal heartbeat is known as the “implantation rate.”
Embryo Grades and Implantation Rates
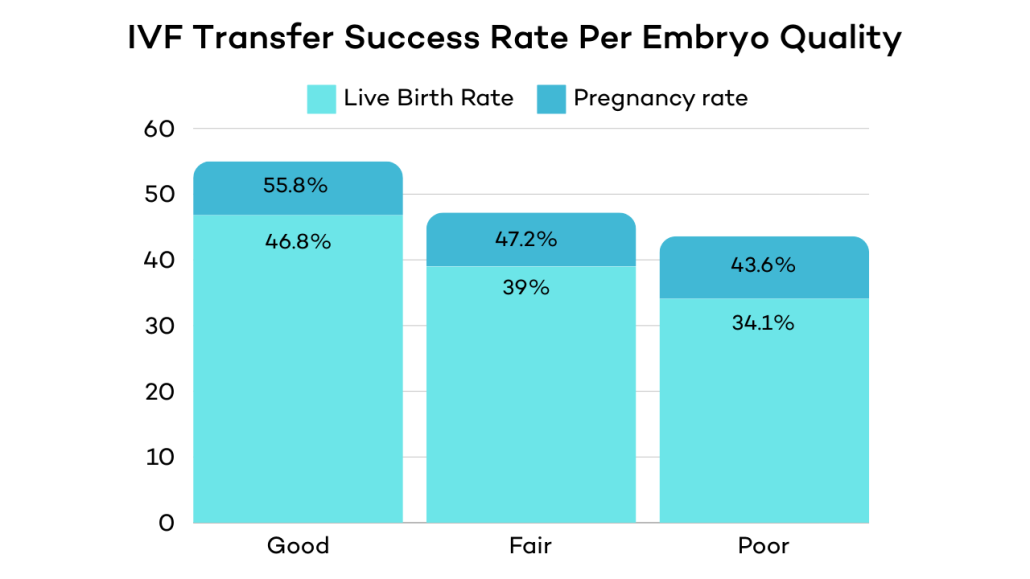
According to a 2017 observational study assessing over 1,700 single embryo transfers, there is a significant relationship between embryo grades and implantation rates [11] :
- “Good” embryos had a 55% implantation rate, and a 46.8% birth rate.
- “Fair” embryos had a 47.2% implantation rate, and a 39% birth rate.
- “Poor” embryos had a 43.6% implantation rate, and a 34.1% birth rate
Keep in mind that a “poor” graded embryo still has a 1 in 3 chance of resulting in a live birth. You can think of it like an A, B, or C grade in school. All are passing grades.
Step 8: Pregnancy Confirmation
Your clinic will administer a blood test to check for pregnancy between 10 and 14 days after an embryo transfer. This is known as the “beta” or “beta hCG.” A number over 100 is considered positive. But more importantly, you want to see your beta hCG level dramatically increase– about double every 29-53 hours. link=”https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6885463/” text=”Revisiting serum β-hCG cut-off levels and pregnancy outcomes using single embryo transfer”/]
Though it’s common to get pregnant with a beta hCG less than 100, beta hCG levels are highly predictive of a successful live birth. For example, a study from 2018 using data from 177 IVF cycles found that [12]
- A day 13 beta hCG under 85 mIU/mL corresponded with an 89% risk of having a miscarriage in the first trimester.
- A day 13 beta hCG greater than 386 mU/mL had a 9% risk of first-trimester miscarriage.
Risk of Miscarriage
The beta hCG test can be one of the most exciting stages of the IVF process, but it’s important to understand your risk of miscarriage.
- A 2018 study found that the overall miscarriage rate for IVF pregnancies was 12.5%. [13]
- The risk of miscarriage increases with age.
- Women between 35 and 45 have a 35% risk of miscarriage.
- Women over 45 have a 50% risk of miscarriage.
- Though these rates of miscarriage can be alarming, studies show that IVF and other fertility treatments are not associated with an increased risk of miscarriage compared with women who conceive naturally. [14]
There are a number of underlying health conditions that can increase the risk of miscarriage, including endometriosis and PCOS. If you’re interested in diving deeper into understanding how your particular health state can affect your likelihood of live birth with IVF, the CDC has created an IVF success calculator.
Overall IVF Success Rates
In 2024, IVF success rates are 32.4% for women between 35 and 37 and 44.5% for women under 35. That’s up from 25.1% for women under 38 in 2001. [15]
Here’s a breakdown of the rates of success for age groups and tested vs. untested embryos.
Chances of untested embryos resulting in a live birth:
- 40% for women under age 35
- 30% for women ages 35-37
- 20% for women ages 38-40
- 10-12% for women ages 41-42
- 5% for women ages 43-44
- Less than 1% for women over 44
Chances of live birth from tested embryos
- 65% regardless of age if the embryo of a PGT tested normal embryo
For success rates between 5%-1%, IVF is no more effective than natural intercourse. Genetic testing is the only assisted reproductive factor that will increase your odds. If you can produce a normal egg and make a normal embryo, genetic testing gives you a 65% chance of pregnancy regardless of age.
Using the IVF Funnel to Understand Your Chances of Success: The Takeaway
IVF has been nothing short of a blessing for millions of families, but it can be a physically, emotionally, and financially demanding journey. Along the way, it’s important to empower yourself by understanding what usually happens along the journey.
Use your knowledge of the IVF funnel as a rough map. There are bound to be blank spots as you explore unknown territory, so be sure to ask your healthcare provider all the questions you need to feel more comfortable and take positive action to increase your odds of success while setting realistic expectations.