IVF With Genetic Testing (PGT): Benefits and Success Rates
This article presents general statistics about IVF success rates to thoroughly discuss and elaborate on preimplantation genetic testing with IVF . The success rates presented are derived from relevant and cited journal articles and are not representative of CNY Fertility’s own clinic data. To view CNY Fertility data, please visit the SART or CDC website.
Genetic testing of embryos can offer empowering insights into the genetic makeup and health of embryos created through in vitro fertilization (IVF). It is also a method for choosing the sex of the child for couples who wish to do so.
In this article, we’ll explore how preimplantation genetic testing is used with IVF and explain the potential of these techniques to increase success rates, choose the sex of your child, and mitigate the risk of specific genetic disorders.
What Kinds of Genetic Testing Are Done With IVF?
Preimplantation Genetic Testing (PGT) is the general term for the genetic testing performed on IVF embryos before the embryo is transferred into the woman’s uterus . PGT is further broken down into three categories:
PGT-A
PGT-A stands for Preimplantation Genetic Testing for Aneuploidy. Aneuploidy refers to an abnormal number of chromosomes in a cell. This is the most common form of PGT, and its primary purpose is to increase the chances of a successful embryo transfer.
A normal embryo has 46 chromosomes. Having more or less than this usually results in failed implantation or early miscarriage. On rare occasions, abnormal chromosomes can lead to genetic disorders such as Down syndrome or Turner syndrome.
When used with IVF, this procedure screens embryos for chromosomal abnormalities before they are transferred to the uterus. Doing so, may increase the chances of successful implantation and reduce the risk of chemical pregnancies and early miscarriage.
The benefits of PGT-A testing are most significant for women of advanced maternal age (35-40+). A large scale 2019 found that PGT did not improve cumulative live birth rates for women under 35 years of age.
PGT-A is also the type of genetic testing that is done to allow patients to choose the sex of their child.
PGT-M
PGT-M stands for Preimplantation Genetic Testing for Monogenic or Single-Gene Disorders. This procedure screens embryos for single-gene disorders that are known to be present in the family.
PGT-M is used by couples who know that they are likely to be carrying specific genetic diseases, and who want to ensure that they do not create offspring with these diseases.
This procedure is often used by couples who may or may not have infertility issues but who wish to increase their chances of having a healthy child.
Here are some specific examples of patients and issues for whom PGT-M is often used.
You and your partner are carriers of the same autosomal recessive condition:
- Cystic Fibrosis
- Sickle cell anemia
- Tay-Sachs disease
You are a carrier of an X-linked condition
- Duchenne Muscular Dystrophy
- Hemophelia B
- Fragile X
You or your partner have an autosomal dominant condition
- Huntington’s Disease
- Neurofibromatosis
- Marfan Syndrome
You or your partner have a mutation associated with hereditary cancer
- BRACA1 & 2 MLH1
- MSH2/6
- PMS1/2 TP53 CHEK2
PGT-SR
PGT-SR stands for Preimplantation Genetic Testing for Structural Rearrangements. This procedure involves analyzing the chromosomes of embryos created through IVF to identify any structural abnormalities such as translocations, inversions, or deletions.
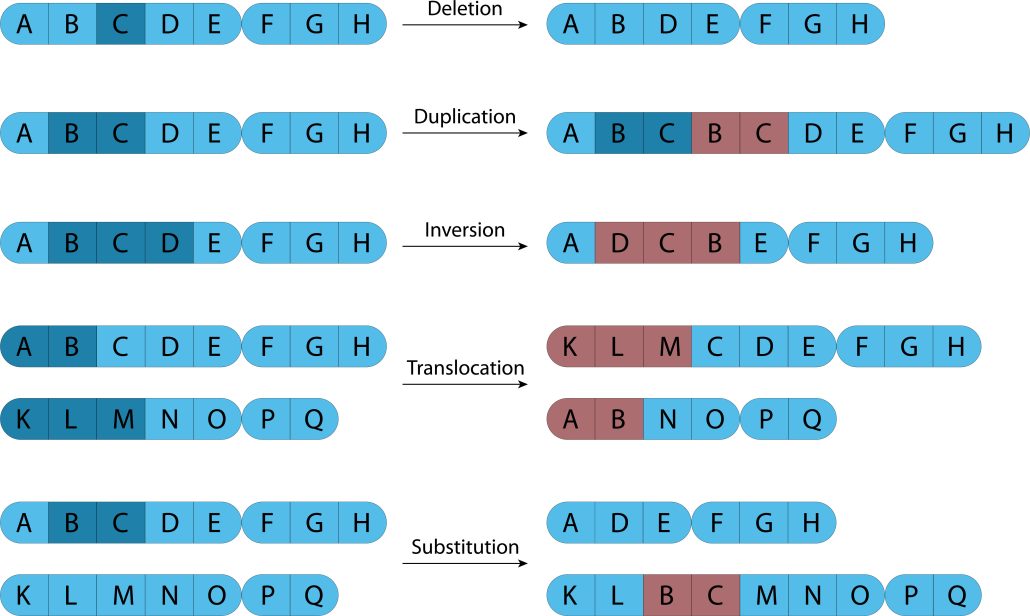
These rearrangements can lead to chromosomal abnormalities in embryos, which may result in miscarriages or genetic disorders in offspring. PGT-SR has been found to be useful for selecting normal or “balanced” embryos for transfer in IVF. Doing so reduces rates of miscarriage.
PGT-A |
PGT-M |
PGT-SR |
|
|
Patient populations |
All IVF populations. Most effective for patients 35-40+ |
At high risk for having a child with a specific genetic disorder |
Patients with structural chromosomal abnormalities |
|
Goal |
Increase chances of a successful pregnancy |
Reduces risk of passing on known inherited condition |
Increase chances of successful pregnancy with normal “balanced” embryos |
|
Test type |
Screens for chromosome abnormalities |
Screens for specific single gene disorder |
Screens for specific unbalanced chromosomes |
The Process of Genetic Testing with IVF
All genetic testing of embryos requires every stage of the IVF process. Here’s a rundown of how it works.
Step 1: Freeze All IVF
You will undergo the initial stages of IVF, including stimulation, egg retrieval, and fertilization of eggs with sperm to create embryos. The embryos will then be grown to the blastocyst stage in a laboratory, usually between days 5-7 after retrieval/fertilization.
Step 2: Embryo Biopsy
Your embryo/s will be biopsied. A small sample (5-10 cells) is taken from the trophectoderm–the part of the embryo that becomes the placenta.
Step 3: Laboratory Testing
The biopsied cells are sent to a genetics lab, where testing is performed.
Step 4: Frozen Embryo Transfer (FET)
Once the testing results are in you will consult with your doctor about the findings. Then, a frozen embryo is selected and thawed for a frozen embryo transfer (FET). Any remaining viable embryos will be frozen for future use or donation.
How successful is IVF with genetic testing?
If you can determine which embryos are genetically normal (known as euploid embryos), a couple is able to increase their odds of a successful transfer and minimize their chances of miscarriage.
Although success rates will vary from patient to patient and clinic to clinic, pregnancy rates generally increase by 10-20% after PGT-A.
Keep in mind that PGT-A doesn’t increase success rates per IVF retrieval; it increases success rates per embryo transfer. PGT-M and PGT-SR are not defined by pregnancy rate but by their effectiveness in detecting genetic disorders.
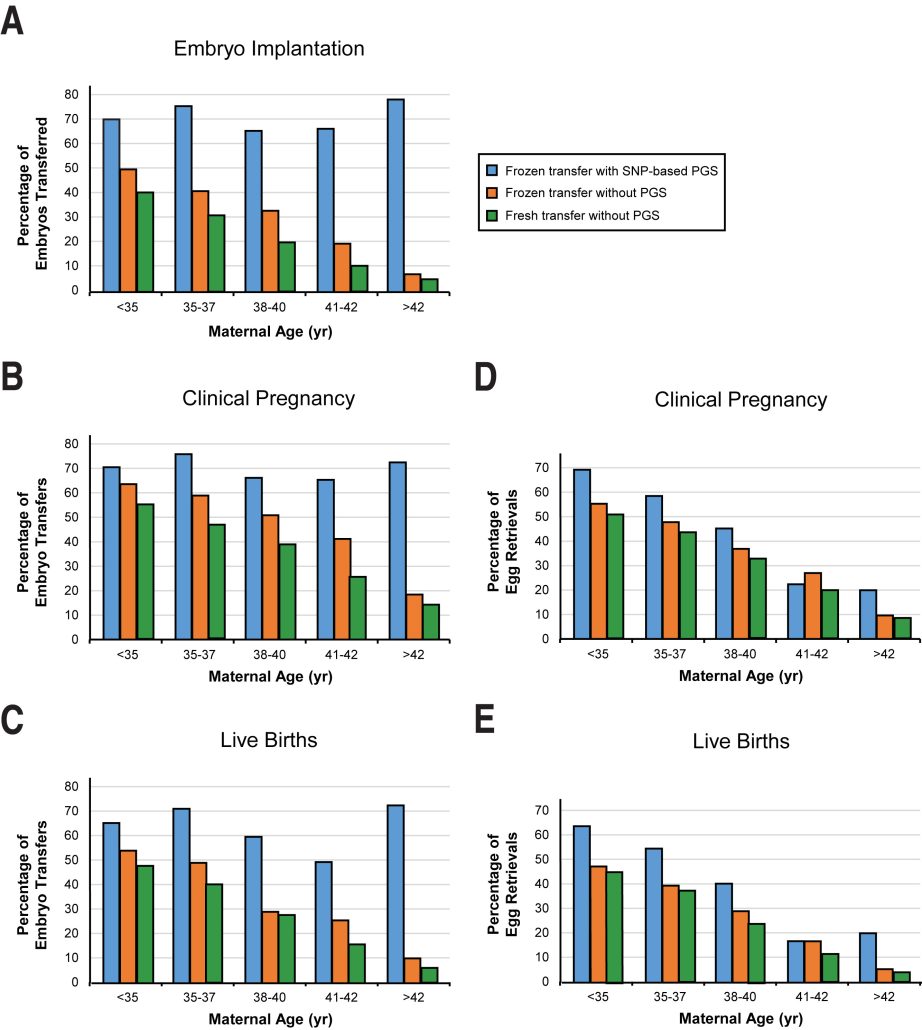
A 2018 study evaluating the effectiveness of SNP-based Preimplantation Genetic Testing for Aneuploidy (PGT-A) in improving IVF outcomes produced the following insights :
High Success Rates
In 1,621 IVF cycles using SNP-based PGT-A the success rates were:
- 69.9% implantation rate (embryos successfully attaching to the uterus)
- 70.6% clinical pregnancy rate per transfer (confirmed pregnancies)
- 64.5% live birth rate per transfer (births resulting from the transfer)
Consistency Across Ages
The success rates of PGT-A were stable across all maternal ages when measured per transfer. However, success rates decreased with age when considering the entire IVF cycle from the beginning.
Low Miscarriage Rates
Women aged 40 and under had low miscarriage rates (about 5%).
Single vs. Double Embryo Transfers
There was no significant difference in pregnancy outcomes between single-embryo transfers (SET) and double-embryo transfers. This suggests that transferring one PFT-A embryo at a time is as effective as transferring two embryos.
Efficiency
On average, it took 1.38 embryo transfers per patient to achieve a live birth.
Overall, the study concluded that PGT-A can mitigate the negative effects of maternal age on IVF outcomes when considering transfer cycles.
Additionally, single-embryo transfers are as effective as double-embryo transfers with PGT-A, supporting the use of SET to reduce risks associated with multiple pregnancies.
In a 2022 study of 430 IVF cycles, researchers found that after transferring embryos created from donor oocytes (eggs), the live birth rate per euploid (normal) embryo was 70.6% (24 out of 34), whereas for untested embryos, it was 34.3% (35 out of 102). This means that there was a 36.3% increase in the live birth rate for genetically tested embryos.
Similarly, after transferring embryos created from eggs that come from the woman’s own ovaries from women who were younger than 35 years at the time of retrieval, the live birth rate per euploid embryo was 70.0% (49 out of 70), compared to 52.5% (53 out of 101) for untested embryos. This means there was a 17.5% increase in live birth rates for genetically tested embryos.

Risks to be Aware of when doing IVF with Genetic Testing
Though genetic testing can be beneficial and even necessary for many people, there are a few risks and limitations to be aware of. These include
Risks and limitations associated with these procedures:
- False positives or negatives can lead to incorrect conclusions about the status of embryos. Embryos affected by genetic abnormalities can still be transferred, while healthy embryos can be discarded. Studies have found an overall accuracy rate of around 90%.
- Embryo damage: There is a small risk of damaging the embryos when removing cells for testing.
- Cost: Genetic testing can add significant cost to the IVF process.
- Limitations: IVF with genetic testing cannot rule out all abnormalities, leaving open the possibility of certain genetic conditions.
- Ethical considerations: Some patients have personal and/or religious concerns about selecting embryos based on genetic criteria.
- Live birth is not guaranteed: Though studies show that genetic testing can significantly increase the rate of live birth, especially for women of older maternal age, there is still no guarantee of success. There are various other factors that impact IVF outcomes and the rates of attrition throughout the process.
IVF with Genetic Testing for Choosing The Sex of Your Child
Gender selection using IVF and Preimplantation Genetic Testing (PGT) is an advanced method with a near 100% accuracy rate.
How much does IVF with Genetic Testing Cost?
The cost of IVF with genetic testing can vary significantly between clinics and depends on the services included in the quoted price.
On average, genetic testing typically adds around $4,500 to the cost of IVF with a Frozen Embryo Transfer (FET), which itself averages around $22,000.
However, at CNY, these prices are considerably lower. Genetic testing, including gender selection, adds closer to $2,000, and IVF with FET totals around $8,000, including the cost of medications. This makes CNY a highly affordable option for those considering genetic testing and gender selection.
IVF with Genetic Testing: The Bottom Line
Genetic testing enhances IVF by reducing genetic risks and increasing pregnancy success rates, particularly for older women.
While it adds costs and presents some limitations, PGT with IVF offers couples more control over family planning, including gender selection. This integrated approach empowers informed decisions, making parenthood dreams more achievable.



