Natural Frozen Embryo Transfer: How It Works
This article presents general statistics about IVF success rates to thoroughly discuss and elaborate on natural frozen embryo transfers. The success rates presented are derived from relevant and cited journal articles and are not representative of CNY Fertility’s own clinic data. To view CNY Fertility data, please visit the SART or CDC website.
Natural cycle frozen embryo transfer (FET) uses the body’s natural hormonal rhythms to guide the embryo transfer process. While medicated FET involves hormone supplementation to prepare the uterine lining, a natural cycle FET is a specialized approach that combines the benefits of a woman’s natural cycle with some medical support.
This method can be effective for women with regular cycles and endometrial lining development who wish to minimize medication use. With close monitoring of ovulation, the embryo is transferred at the precise time when the uterus is naturally optimal for implantation. This process reduces the need for additional hormonal medications and aligns implantation with the body’s inherent timing.
What is Natural Frozen Embryo Transfer
A natural frozen embryo transfer (FET) is a procedure in which a frozen embryo from a previous IVF cycle is thawed and then transferred into the uterus during the natural implantation window in the luteal phase. In this approach, the transfer is timed from ovulation when the lining of the uterus (endometrium) is naturally primed with the body’s own progesterone for implantation.
Natural FET is done without the use of some hormonal medications that are typically used in medicated cycles to prepare the lining of the uterus in a way that mimics the natural cycle.
The Natural Frozen Embryo Transfer Process and Timeline
A Natural Frozen Embryo Transfer takes place using a frozen embryo from a previous IVF cycle and includes the following additional steps.
Cycle Day 1: Menstrual Cycle Begins
- The natural FET process begins on the first day of the menstrual period.
Cycle Days 10-14: Ovulation Monitoring
- The woman’s menstrual cycle is closely monitored to track endometrial lining development and natural ovulation. Typically, this entails regular ultrasound scans and blood tests to measure the uterine lining and check hormone levels. You may also be required to take ovulation predictor tests (OPKs) at home so ovulation is not missed.
Cycle Days 14-16: Ovulation Detection
- A surge in LH levels or the release of the egg visualized via ultrasound confirms ovulation. Once ovulation is detected, the timing for the embryo transfer is scheduled.
Cycle Days 17-20: Embryo Thawing and Transfer
- The embryo transfer is scheduled for 3 to 5 days after ovulation, depending on the age of the embryo. On the day of transfer, embryos that were frozen during a previous treatment cycle are thawed in a lab and transferred into the uterus using a long catheter.
Cycle Days 29-31: Pregnancy Test
- Around 9-11 days after the embryo transfer, a blood test is performed to check for pregnancy by measuring hCG levels. This is called the “beta” or “beta hCG.” A value of 5 or above is considered positive. More importantly, you will want the beta hCG level to increase. Ideally, you will want this number to double every 48 hours.
Modified Natural Frozen Embryo Transfer
A modified natural frozen embryo transfer is any non-standardized variation of the natural FET.
A modified natural FET is different from a completely natural FET in that it includes minimal use of medications to support and optimize the natural cycle.
A typical modified natural FET can look like this:
- Cycle monitoring is similar to a natural FET. Ultrasound scans and blood tests are used to track ovulation. Sometimes a medication called letrozole will be used to help you to grow an egg, and in turn, grow the uterine lining.
- Ovulation support: A trigger shot of human chorionic gonadotropin (hCG), leuprolide acetate (Lupron), or a combination of both may be given to induce ovulation at a specific time in alignment with the natural cycle. The use of a trigger shot allows better control of the timing of the ovulation and embryo transfer.
- Luteal phase support: Your fertility specialist may prescribe a progesterone supplement to optimize the uterine lining for implantation during the luteal phase. This includes the days following the trigger shot/ovulation and leading up to the embryo transfer/potential implantation.
- The embryo transfer process takes place 3-5 days after trigger/ovulation and is identical to a natural FET.
- Post-transfer support and monitoring: After the transfer you may continue taking progesterone in the form of a vaginal suppository and possibly other medications to support the early stages of pregnancy.
Natural Frozen Embryo Transfer Success Rates
Natural Frozen Embryo Transfer (FET) success rates vary but are generally comparable to those of medicated cycles. Success depends on factors like the woman’s age at the time the eggs were retrieved, embryo quality, and overall health.
Many clinics report success rates ranging from 30% to 50%, with slightly higher rates for younger women and higher-quality embryos. Here’s a rundown of the current research.
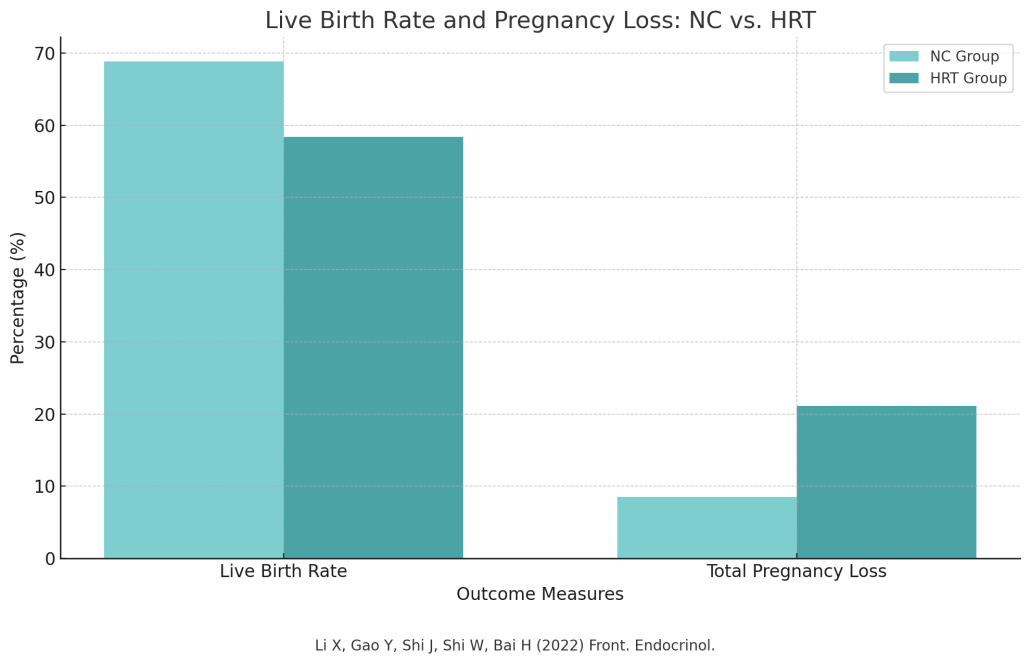
In a 2022 study examining 598 single natural frozen embryo transfers researchers found that women undergoing natural frozen embryo transfers had better outcomes compared to those using programed/medicated FETs.
The natural transfer group had a significantly higher live birth rate (68.8% vs. 58.35%) and a lower risk of total pregnancy loss (8.51% vs. 21.14%).
In a 2023 study, 1,428 women were randomly assigned to three groups: natural cycle, modified natural cycle, and artificial cycle.
Researchers found that 99 first FET cycles were canceled in both the natural and modified cycle groups, but none were canceled in the artificial cycle group.
The live birth rates after one FET were similar across all three groups: 37% for the natural cycle, 33% for the modified natural cycle, and 34% for the artificial cycle. The study found no significant differences in maternal and neonatal outcomes between the groups.
A 2023 meta-analysis looking at neonatal outcomes for natural vs. artificial cycle FET found that that using natural cycle frozen embryo transfer (NC-FET) can significantly reduce the risk of adverse obstetric and neonatal outcomes compared to artificial cycle FET (AC-FET).
The researchers estimate that for every 1,000 women, natural cycle FET may prevent 4 to 22 cases of adverse outcomes. The researchers concluded that natural cycle FET should be the preferred approach for women with regular ovulatory cycles undergoing FET.
Why Choose Natural FET?
There are various reasons why clients choose natural FET. Some of the most common reasons include:
- Less medications: By eliminating medications and relying on the body’s natural processes there are no side effects.
- Comparable success rates: Research indicates that the success rates to medicated FET cycles.
- Reduced cost: Medications are a significant expense and reducing medications lowers the total cost of treatment.
Limitations of Natural Frozen Embryo Transfer
To be able to do a natural cycle FET, woman must have ovarian function, ovulate normally during regular menstrual cycles between 21 and 35 days, or be able to respond to letrozole.
Planning a natural FET can be more complex and might involve additional monitoring. For example, instead of using ovulation kits, a doctor may choose to closely monitor LH levels through blood tests, and more ultrasounds might be necessary to track the development of the follicles.
Natural Frozen Embryo Transfer: The Takeaway
Natural cycle frozen embryo transfer (FET) offers a less medicated approach to fertility treatment, aligning with the body’s natural hormonal rhythms.
It can be a highly effective option for women with regular cycles, providing comparable success rates to medicated cycles while reducing the need for additional medications and lowering the risk of adverse outcomes. While it may require more monitoring, the benefits make it a preferred choice for many.
If you’re interested in seeing if you’re a good candidate for a natural or modified natural FET as part of your IVF journey, schedule a consultation with one of our fertility specialists today.

