Preimplantation Genetic Diagnosis (PGD)
As any person undergoing or considering fertility treatment can tell you, trying to understand all of the fertility acronyms and language is like learning a new dialect. For this article, we are going to try and simplify the language around the genetic testing of embryos and explain in detail a type of embryonic testing often referred to as Preimplantation Genetic Diagnosis (PGD).
What is PGD?
Preimplantation genetic diagnosis, or simply PGD, is a reproductive technology used alongside In Vitro Fertilization (IVF) to test the genome of IVF embryos prior to being transferred into the woman’s uterus. PGD helps couples at risk of having children with a specific genetic condition and those with chromosomal rearrangements have healthy pregnancies and unaffected children. In this fashion, PGD could be thought of similarly to prenatal genetic testing, only the testing is done on a 5-day old embryo rather than a growing fetus; this helps avoid unnecessary pregnancy loss or selective abortions.
The PGD procedure begins with the normal IVF process – ovarian stimulation, egg retrieval, and fertilization and embryo development in a laboratory. However, after embryos reach the blastocyst stage, a few cells are removed from the embryo for genetic testing while the embryos are frozen to await the testing results. These cells are sent to a genetic testing lab to check for chromosome anomalies or certain genetic mutations. Preimplantation Genetic Diagnosis is completed prior to embryo implantation to help identify specific genetic abnormalities and conditions that could affect the success of IVF and the health of the future baby. This helps hopeful parents with known genetic abnormalities to comfortably and safely have a safe pregnancy resulting in a healthy child by select the best embryo to transfer.
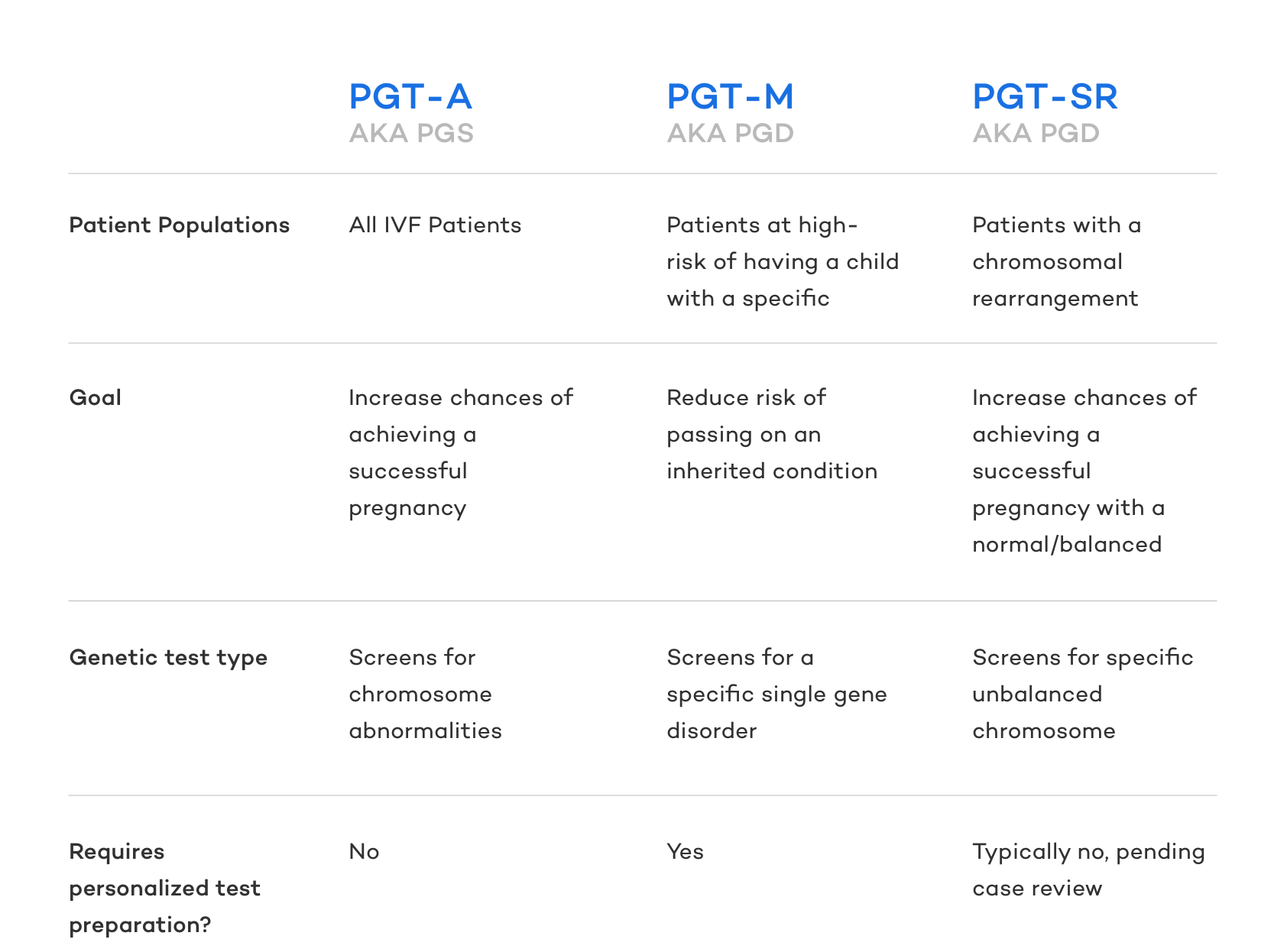
Interesting enough, Preimplantation Genetic Diagnosis is actually an out of date term. The medical community has adopted new terminology for PGD as a way of alleviating confusion as PGD described two significantly different genetic tests. Preimplantation Genetic Diagnosis is now broken into two terms to describe these unique tests:
- PGT-M (pre-implantation genetic testing monogenic/single gene defects): Reduces the risk of passing on a known genetic abnormality (ie. sickle cell anemia, cystic fibrosis, muscular dystrophy, Huntington’s disease).
- PGT-SR (pre-implantation genetic testing chromosomal structural rearrangements): increase the odds of a normal pregnancy of someone with a known chromosomal rearrangement.
There is indeed another very common type of embryonic genetic testing done during IVF known as Preimplantation Genetic Screening (PGS – old terminology) or Preimplantation Genetic Testing for Aneuploidy, but as this is another unique type of test and was never classified as PGD, we will not be discussing it further in this article.
That said, PGD is still widely used by both fertility patients and specialists alike so we will use the term PGD frequently in this article. We will however specify which form of PGD (PGT-M or PGT-SR) we are referring to when necessary.
PGD as PGT-M
PGT-M is a genetic test designed to reduce the risk of having a child with an inherited condition. PGT-M testing is completed during the IVF process after the eggs have been fertilized and have developed into embryos. PGT-M is performed prior to establishing pregnancy through the embryo transfer portion of the IVF process to reduce the risk of having a child affected by a single gene disorder. After PGT-M testing is completed, embryologists can easily identify unaffected embryos that will provide the best chances for a successful and healthy pregnancy.
Examples of single-gene disorders that PGT-M screens for are sickle cell anemia, cystic fibrosis, and Duchene muscular dystrophy . A majority of single-gene disorders are considered rare, but they still affect millions of Americans. Luckily, PGT-M can screen for over 6,000 single-gene disorders.
Who should consider the PGT-M version of Preimplantation Genetic Diagnosis
PGT-M is recommended for patients who have undergone genetic screening and learned of their risk status for passing on a specific genetic condition because of the following:
- Both partners are carriers of the same autosomal recessive condition (i.e. Tay Sachs Disease)
- Either partner is a carrier of an X-linked condition (i.e. Hemophilia A)
- One or both partners have an autosomal dominant condition (i.e. Huntington’s disease)
- One or both partners have a mutation associated with a hereditary cancer syndrome (i.e. BRCA1 & 2)
PGT- M testing is also recommended for patients who have a known genetic mutation in either their or their partner’s family or who have previously had a child or pregnancy with a single gene disorder.
How PGD as PGT-M Works
Genetic testing of embryos is more complicated than genetic testing of a blood sample due to the small amount of DNA available. PGT-M is most commonly completed via a technique called karyomapping. Karyomapping is a genetic mapping technology that maps hundreds of thousands of data points across the entire genome and subsequently performs a linkage analysis.
In karyomapping, DNA samples are collected from the sperm and egg providers, as well as from family member(s) who are known to be gene carriers or non-carriers. The samples are examined to identify the chromosomal location of gene mutation(s) in the family. Based on these results, embryos are tested to see if they carry “normal” genes or genes with the mutation(s). Karyomapping has improved the accuracy of PGT-M and has shortened the test preparation process. Research has shown that karyomapping is highly accurate and allows for analysis of the inheritance of almost any single-gene defect .
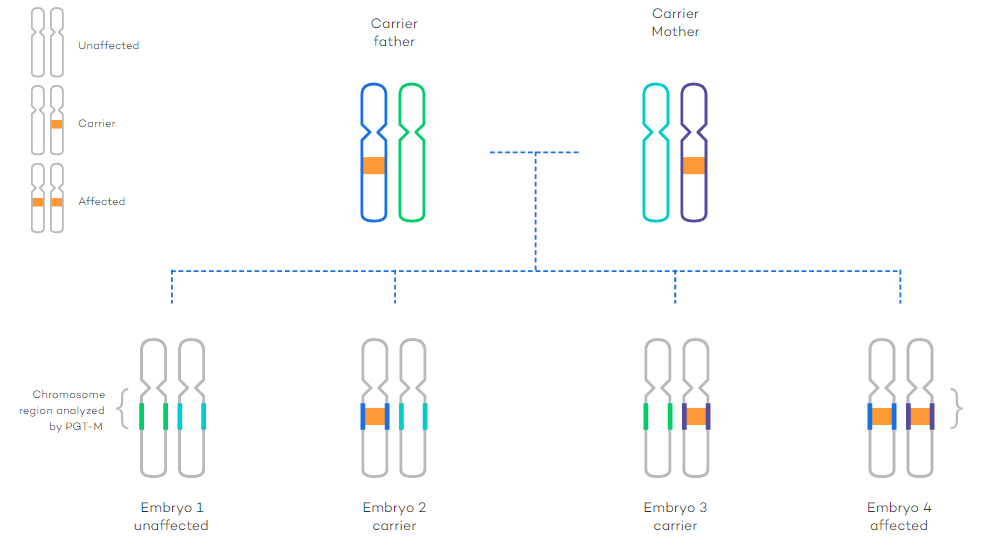
PGT-M testing examines both the mutation an individual carries and the area of the chromosome surrounding it. These areas are represented by the colored segments in the figure below.
What are the Steps of PGT-M
Prospective patients begin by speaking with a genetic counselor to determine if additional genetic testing is required for the couple or other family members. After the initial case review, the PGT-M laboratory will design unique tests. Each PGM-T test is specifically designed and tailored to the individuals being tested. As such, DNA samples from both partners (and often additional family members) are required to design the test.
Couples must then undergo IVF to create embryos for testing. After the egg retrieval and fertilization, the embryos are incubated for 5-6 days after retrieval until they reach the blastocyst stage. Embryos that reach the blastocyst stage have a higher chance of implantation when they are transferred into the uterus.
After embryos reach the blastocyst stage, embryologists remove a small cell sample from each embryo produced via IVF. After the sample is removed, the embryos are frozen. The embryo samples are sent to a PGT-M laboratory and the specifically designed testing is completed.
The PGT-M lab sends the results of the tests back to the fertility clinic. The fertility clinic will then contact the patients to discuss the results of the test. Based on the results of the test, the embryologist selects the best of the unaffected embryos for transfer. When the female is ready, the embryo can be thawed and transferred into the woman’s uterus. The remaining embryos will remain frozen until they are needed in the future. Any affected embryos with the genetic abnormality are usually discarded.
PGD as PGT-SR
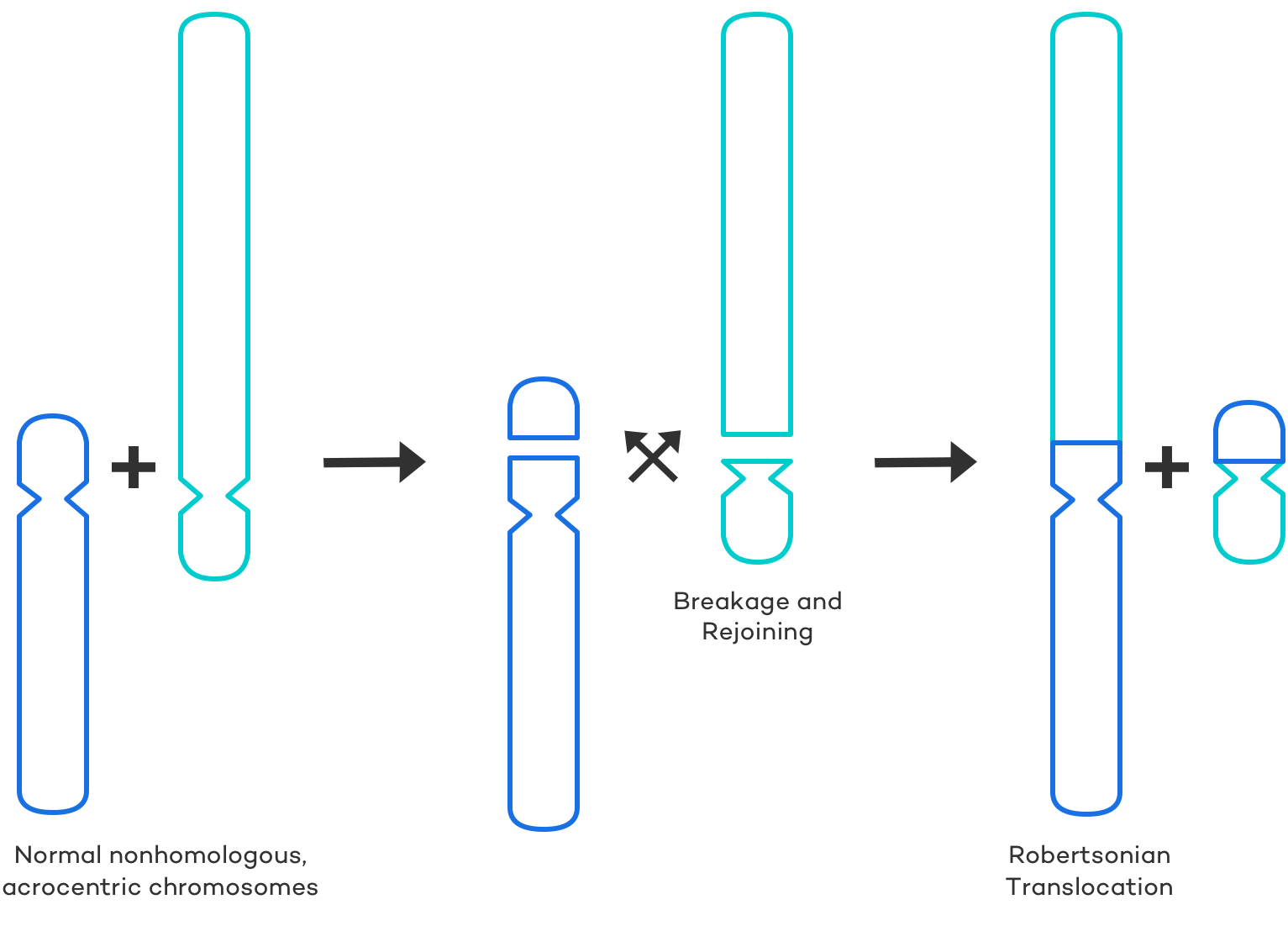
PGT-SR is a genetic test that can determine whether embryos created through IVF have chromosomal rearrangements. Chromosomes are the structures that hold our genetic material. Chromosomal rearrangements happen when changes occur to the normal size or arrangement of chromosomes. Chromosome rearrangements can be inherited or can happen via a spontaneous mutation. PGT-SR can identify both types of rearrangements. By identifying chromosomal rearrangements prior to implantation, technicians can choose the best embryos to maximize the chances of a successful pregnancy. Types of chromosomal rearrangements include:
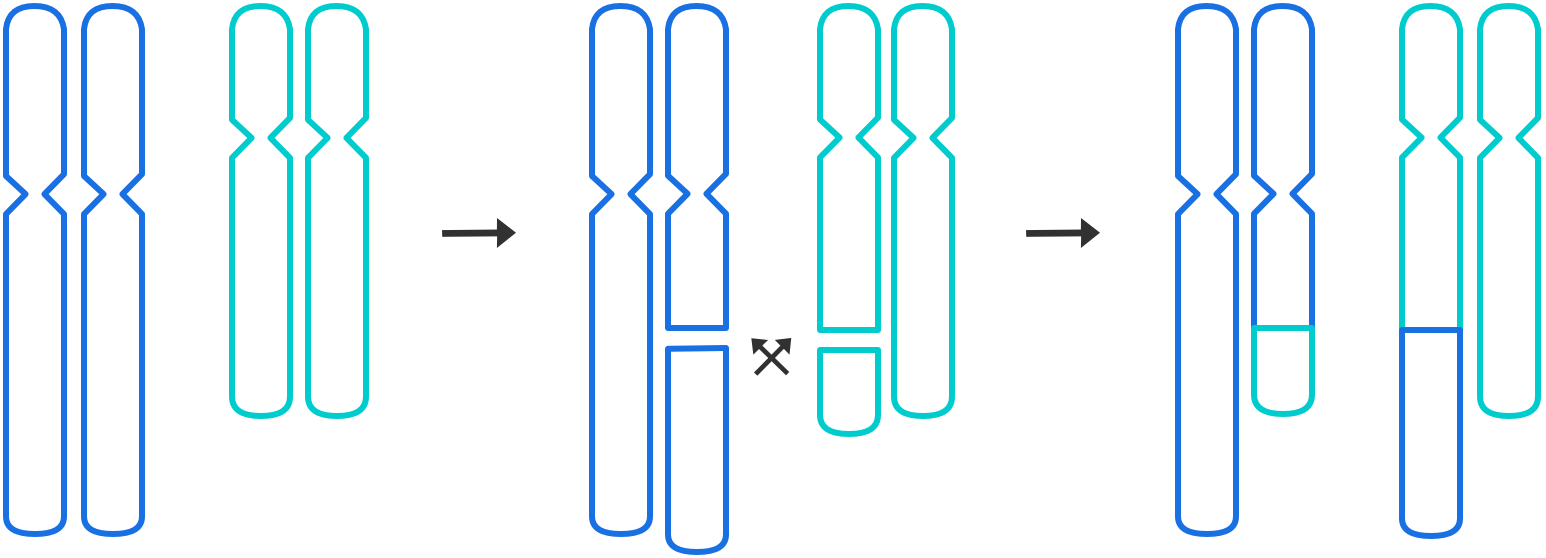
- Translocations: occur when segments of two chromosomes break off and change places
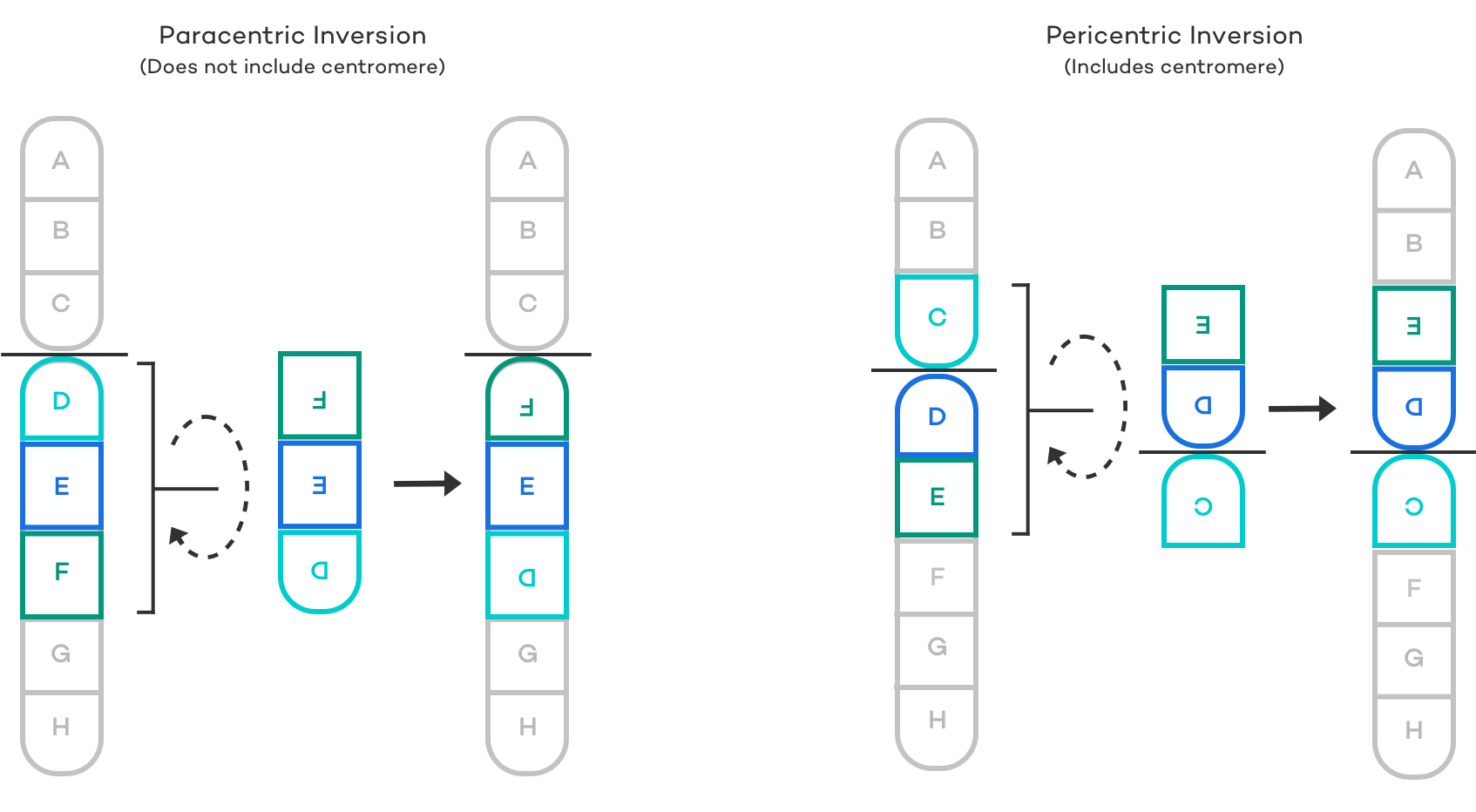
- Inversions: occur when a segment of a chromosome has reversed orientation
- Deletions: occur when a segment of a chromosome is missing
- Duplication: is when there is an extra segment of a chromosome
- Insertion: occurs when a segment of a chromosome has been inserted into the incorrect location
Individuals whose chromosomes have a balanced translocation or inversion have all the correct genetic information; however, sections of their genetic material are found in a different location or position than normal. Usually, these individuals are healthy and are unaware of their carrier status until they try to have children. These individuals are at an increased risk for infertility, miscarriage, and/or passing along that chromosome abnormality to their child.
Who should consider the PGT-SR version of Preimplantation Genetic Diagnosis
PGT-SR is recommended for people who have undergone a karyotype (chromosome study on blood) and are known to have a chromosome rearrangement. It is also recommended for people who have previously had a child or pregnancy with a chromosome rearrangement. PGT-SR should be considered by anyone who is at risk of creating embryos with an incorrect chromosome number or structure and it is available for most inherited structural chromosome abnormalities.
You may consider PGT-SR for chromosome rearrangements if you or your partner are a carrier of any of the following:
Inversions:
Inversions are chromosomal rearrangements that involve only one chromosome. In an inversion, a segment of a chromosome is flipped and reinserted upside down.
Inversions look something like this . . .
Reciprocal translocations:
Robertsonian translocations:
How PGD as PGT-SR Works
Most genetic testing laboratories offer several different technologies for PGT-SR for chromosomal rearrangement depending on the specific case and the fertility clinic’s preference. PGT-Sr tests embryos for both inherited and spontaneous chromosomal rearrangements. Patients that are known carriers of balanced rearrangements are at risk for producing embryos with the incorrect amount of chromosomal material. Affected embryos are less successful in achieving pregnancy than embryos that have been screened and cleared as having the normal amount of chromosomal material. PGT-SR helps to identify embryos with the correct amount of chromosomal material increasing the chances of a successful pregnancy and live birth.
What are the Steps of PGT-SR
Similar to PGT-M testing, the PGT-SR process starts with the prospective patient(s) speaking with a genetic counselor. After the prospective patients complete their fertility testing with their fertility clinic, then their case will be reviewed by the PGT lab. Next, the patient will undergo the stimulation and retrieval portion of the IVF process to produce embryos for testing. Embryos are then fertilized using either IVF or ICSI. The embryos are then incubated for 5-6 days until they reach the blastocyst stage. The embryologist will then complete an embryo biopsy and remove 5-10 cells from each embryo. The embryos are then frozen until they are needed for transfer. The embryo biopsy samples are then sent to the PGT lab where testing is conducted.
The PGT lab will perform genetic testing for both sporadic and inherited chromosomal rearrangements. PGT-SR screens out embryos that carry unbalanced translocations, ensuring only embryos with the correct amount of genetic material are selected for transfer. The PGT lab will communicate the results of the chromosome analysis with the fertility clinic. The embryologist at the fertility clinic will select the best of the normal embryos to be transferred into the patient’s uterus. The additional normal embryos are stored for future use.
Frequently Asked Questions about PGD
Who should consider Preimplantation Genetic Diagnosis?
- People who have a known chromosome rearrangement and are at risk of creating embryos with the incorrect chromosome number or structure
- People who have had a child or pregnancy with a chromosome rearrangement or a specific gene disorder
- People who are carriers of an inversion, reciprocal translocation, or Robertsonian Translocation
- Couples where both partners are carriers of the same autosomal recessive condition (e.g. Cystic fibrosis)
- People who are carriers of X-linked conditions (e.g. Duchenne Muscular Dystrophy)
- People who have an autosomal dominant condition(s) (e.g. Huntington disease)
- People who have a mutation associated with a hereditary cancer syndrome (e.g. BRCA1 & 2)
- People who want to perform HLA matching
Are embryos genetically modified using PGD?
Embryos are not genetically modified using PGD. Nothing is added to embryos during the PGD process, they are simply screened for genetic abnormalities to increase the chances of successful IVF. The embryos themselves are not affected in any way besides the small number of cells removed during the blastocyst stage for the endometrial biopsy.
How are embryos chosen for transfer?
PGD testing identifies embryos that are genetically normal and abnormal. The PGD lab sends the results of the test to the fertility clinic where the embryos are frozen. Based on the results of the PGD, the embryologist will separate the normal and abnormal embryos. Embryologists grade embryos in the blastocyst stage based on three criteria; the degree of expansion based on how expanded the cavity is, the appearance of the inner cell mass, and the appearance of the trophectoderm. The highest graded normal embryo is chosen for transfer.
Check out our Embryology FAQ page for more information on grading embryos.
Where does Preimplantation Genetic Diagnosis occur?
After embryos are collected during IVF, they are fertilized and incubated in the embryology lab until they reach the blastocyst stage. After embryos reach the blastocyst stage, they are biopsied (a small section of the embryo that becomes the placenta is removed). The biopsied cells are then sent to a genetics laboratory (offsite from the fertility clinic) and genetically screened.
Is embryo biopsy and PGD safe? What are the concerns or risks of PGD?
Research has shown that PGD testing of blastocysts ensures accuracy, reliability, and reproducibility for results and shows no impact upon embryo viability and reproductive potential . The major downside of a PGD biopsy is that it cannot be completed along with a fresh embryo transfer. Embryos that undergo PGD testing must be frozen and later transferred through a frozen embryo transfer.
The use of a frozen embryo transfer is only considered a disadvantage if the patient prefers to transfer a fresh embryo. In fact, research has indicated that frozen embryo transfers may result in higher cumulative live birth rates compared to fresh transfers . During a fresh transfer, women’s bodies don’t have much time to recover from the ovarian stimulation phase leading up to their retrieval. Undergoing a frozen transfer allows women’s bodies more time to recover which allows progesterone and estrogen levels to balance out and their endometrial lining to become more receptive.
Is Prenatal Testing Still Necessary After PGD?
Prenatal testing is absolutely still recommended after PGD. Although slim, there is still a chance that your baby can suffer from a birth defect as a result of a genetic disorder even after PGD. PGD does not guarantee the birth of a chromosomally normal child due to the risk of undetected mosaicism. Mosaicism is a condition in which cells within the same person have different genetic makeup. As such, fertility specialists recommend that patients who complete IVF with PGD undergo prenatal testing between weeks 10 and 12 of pregnancy.
You can learn more about the risk of PGD here.
The Bottom Line about PGD
Pre-implantation genetic diagnosis (PGD) is a wonderful resource for patients who are known to be at risk for passing on a chromosomal abnormality or who have a chromosomal rearrangement and plan to undergo IVF treatment. PGD testing presents virtually no risk to blastocyst embryos and in addition to reducing the risk of passing along a genetic condition to a future child, PGD can also increase the likelihood of success with IVF. After PGD testing, embryos are thawed and transferred via a frozen embryo transfer. Frozen embryo transfers may also provide women with improved chances of achieving pregnancy because their bodies have more time to recover following their retrieval and ovarian stimulation.
For more information on improving your chances of success with IVF, check out our articles on naturally improving fertility, what foods to eat when trying to get pregnant, and our male and female-specific fertility-boosting guides.


