What is a Saline Infusion Sonohysterogram (SHG)? Everything You Need to Know
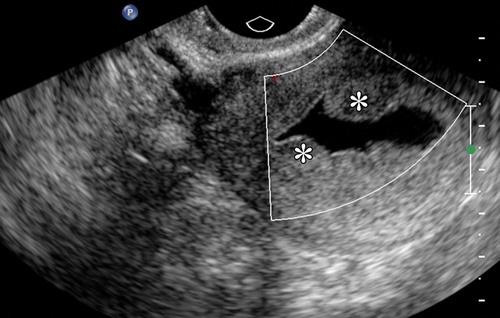
A Saline Infusion Sonohysterogram (SHG) can be an important diagnostic tool that most fertility clinics use as part of their standard preconception testing regimen. This minimally invasive protocol involves introducing sterile saline into the uterine cavity, followed by transvaginal ultrasound imaging. After the saline expands the uterine cavity, the ultrasound can provide a detailed view of the uterus’s lining and the ovaries.
As a standard part of preconception testing before beginning most fertility treatments, SHG is used to identify conditions such as polyps, fibroids, adhesions, and congenital abnormalities that could affect implantation and, therefore, the success rates of various assisted reproduction technologies such as IUI and IVF.
In this article, we will explore the use of SHG in assisted reproduction, including when it is used, the benefits, and risks to look out for.
What is a Saline Infusion Sonohysterogram (SHG)?
A Saline Infusion Sonohysterogram (SHG) is an ultrasound technique used to examine the interior of the uterus.
An SHG involves introducing a small amount of sterile saline solution into the uterine cavity via a thin catheter. This saline solution helps to expand the uterine cavity, which allows for better visualization of the endometrial lining during the ultrasound examination.
When is an SHG Performed?
An SHG- between cycle days 5-10. This is early in the cycle when the lining is at its thinnest and there is a low likelihood of uterine bleeding.
Why is an SHG Performed?
There is a wide variety of uterine abnormalities that can impair fertility. Many of these, including common abnormalities like polyps and fibroids, are often too subtle to detect with a standard ultrasound.
For this reason, the enhanced resolution of a saline infusion sonohysterogram is a required feature of a comprehensive evaluation of the uterus before making a diagnosis or developing a fertility treatment plan.
At CNY Fertility, an SHG is part of the required preconception testing that must be completed prior to any female fertility treatment.
What Conditions Does an SHG Look for?
An SHG can be done to investigate various conditions that can impair female fertility and cause recurrent miscarriages. Some of the primary conditions include:
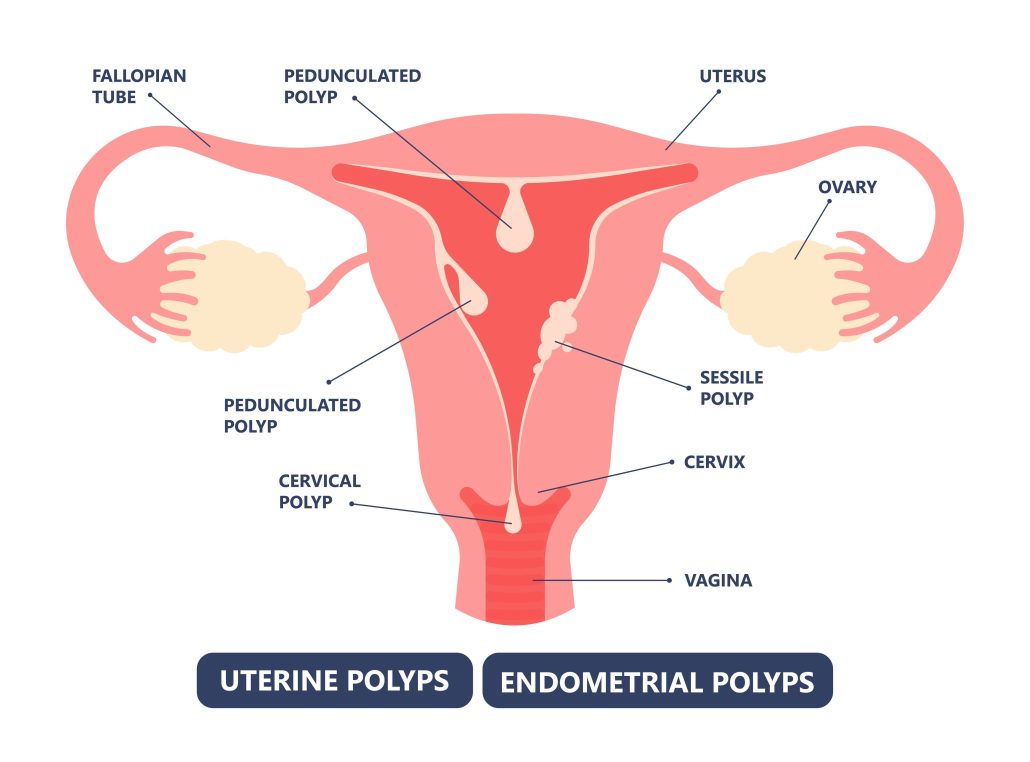
Uterine Polyps
Small, benign overgrowths on the lining of the uterus (endometrium). Polyps can cause irregular menstrual bleeding and may interfere with fertility by affecting embryo implantation.
One study found polyps in 32% of patients (323/1000) undergoing IVF. Polyps have been found to be the most common uterine abnormality in patients with recurrent implantation failures after IVF, affecting 16.7 % of this population.
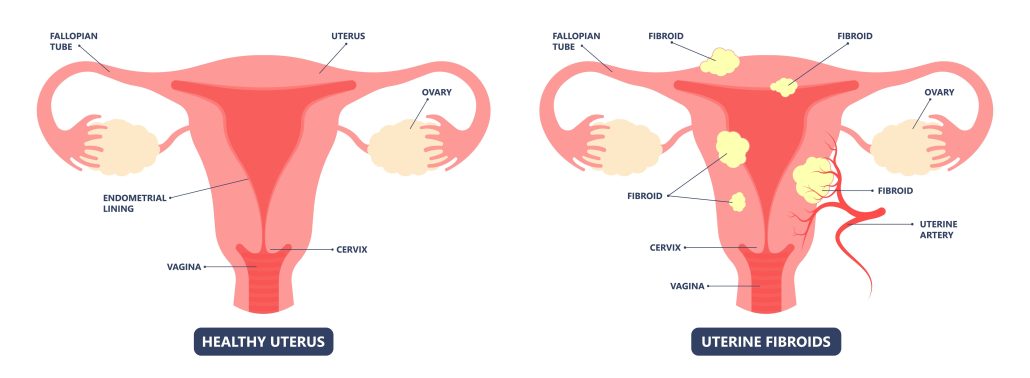
Uterine Fibroids
Non-cancerous fibrosis (hard) growth that can form within or outside of the muscle tissue of the uterus. Fibroids can distort the uterine cavity, cause heavy menstrual bleeding, pain, and potentially impact fertility.
A 2012 study found that uterine fibroids affect between 35-77% of women of reproductive age.
Endometrial Adhesions (Asherman’s Syndrome)
Characterized by bands of scar tissue inside the uterine cavity, resulting most often from previous surgery or infection.
These adhesions can cause menstrual irregularities and pelvic pain. These adhesions can impair fertility by impeding the transportation of sperm, causing embryo implantation to fail, and interfering with the formation of the placenta.
Congenital Uterine Anomalies
Various uterine abnormalities can be present from birth. Two common abnormalities are a septate uterus (a wall dividing the uterine cavity) and a bicornuate uterus (a heart-shaped uterus).
These abnormalities can lead to failed implantation during IUI and IVF procedures and increase the risk of miscarriage and complications during pregnancy.
Submucosal Fibroids
Submucosal fibroids can originate from the innermost layer of the uterine muscle or extend from other layers, exhibiting submucosal components. They can buldge into the uterine cavity. Despite being benign, these tumors can undergo rapid growth, lead to heavy menstrual bleeding, and may interfere with fertility.
Studies have found that they become symptomatic in around 30% of women and are the most common reason for hysterectomies that prematurely end a woman’s reproductive potential. These negative outcomes make an SHG a critical tool for early diagnosis of this potentially devastating condition.
The Takeaway
Overall, an SHG provides crucial information that helps accurately diagnose various causes of infertility, allowing specialists to tailor treatments to individual needs.
How is SHG performed?
Here’s a step-by-step summary of how the SHG procedure is performed:
- A speculum is inserted into the vagina to help with the visualization of the cervix
- A thin, flexible catheter is gently inserted through the cervix into the uterine cavity.
- A sterile saline solution is slowly infused through the catheter into the uterine cavity. The speculum is removed.
- The saline expands the cavity, creating a better view of the uterine walls and lining.
- An ultrasound probe is inserted into the vagina.
- The saline acts as a contrast medium, improving the visibility of the endometrial lining and any abnormalities.
SHG is commonly used to evaluate abnormal uterine bleeding, investigate infertility issues, and diagnose potential uterine abnormalities. It is a minimally invasive procedure, generally well-tolerated by patients, and carries a low risk of complications. The enhanced visualization provided by SHG allows for a more accurate diagnosis than a traditional ultrasound, making it an essential tool in gynecological and reproductive health.
Safety, Side Effects, and Contraindications of an SHG
An SHG is considered minimally invasive and very safe.
The main contraindications for an HSG are pregnancy, STIs, and active pelvic inflammatory disease (PID). If a client has no known PID but engages in high risk behavior that would put her in a position to have STI’s it is still contraindicated.
Complications are rare but can include a vasovagal response (heart rate and blood pressure to suddenly drop, 4.1%), pelvic pain (3.8%), post-procedural nausea (1%), and fever (0.8%).
Additionally, SHG can sometimes lead to cramping, spotting, and vaginal discharge. Some women may experience cramping for several hours following the procedure.
It is generally advised to take a pain reliever like ibuprofen beforehand. In some cases, doctors might prescribe stronger pain medications or antibiotics before the SHG. You should contact your doctor if you experience pain or fever within 1–2 days after the procedure.
Saline Infusion Sonohysterogram (SHG): The Takeaway
A Saline Infusion Sonohysterogram (SHG) is an essential diagnostic tool for those experiencing infertility or otherwise seeking fertility care.
This minimally invasive procedure enhances the visualization of the endometrial lining and detects uterine abnormalities through transvaginal ultrasound.
SHG is particularly useful in identifying conditions such as polyps, fibroids, adhesions, and congenital abnormalities that could impact fertility treatment, including implantation and the success rates of IUI, IVF, and other assisted reproductive technologies.
The procedure is relatively simple and well-tolerated, providing crucial information for tailoring fertility treatments to individual needs. By ensuring a thorough evaluation of the uterine environment, SHG helps fertility specialists make informed decisions and improve the chances of successful pregnancy outcomes.

